Cardiology
Cardiology 2
752 - Getting Through the Night: Understanding ‘In-the-Moment’ Resilience of Pediatric Cardiology Fellows in the Cardiac Intensive Care Unit
Publication Number: 752.304

Priya Misra, MD (she/her/hers)
Pediatric Cardiology Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Many studies have highlighted the prevalence and negative impact of physician burnout, but there are few that focus on understanding and promoting resilience, especially in physician trainees.
Objective:
Our primary objective was to understand what contributes to ‘in-the-moment’ resilience for pediatric cardiology fellows while on-call in the Cardiac intensive Care Unit (CICU). Our secondary objective was to identify potential interventions to enhance physician resiliency and patient safety.
Design/Methods: This is an IRB-exempt, multi-center, mixed-methods study. The qualitative data consisted of semi-structured, in-depth, individual interviews with categorical pediatric cardiology fellows from two training programs. Transcripts were coded and analyzed using the phenomenology tradition through an inductive approach with the lens of “protective” and “compensatory” conceptual frameworks for resiliency, until thematic sufficiency was obtained. Quantitative data included baseline demographics, an evidence-based two-question burnout screen and quantification of negative effects from call.
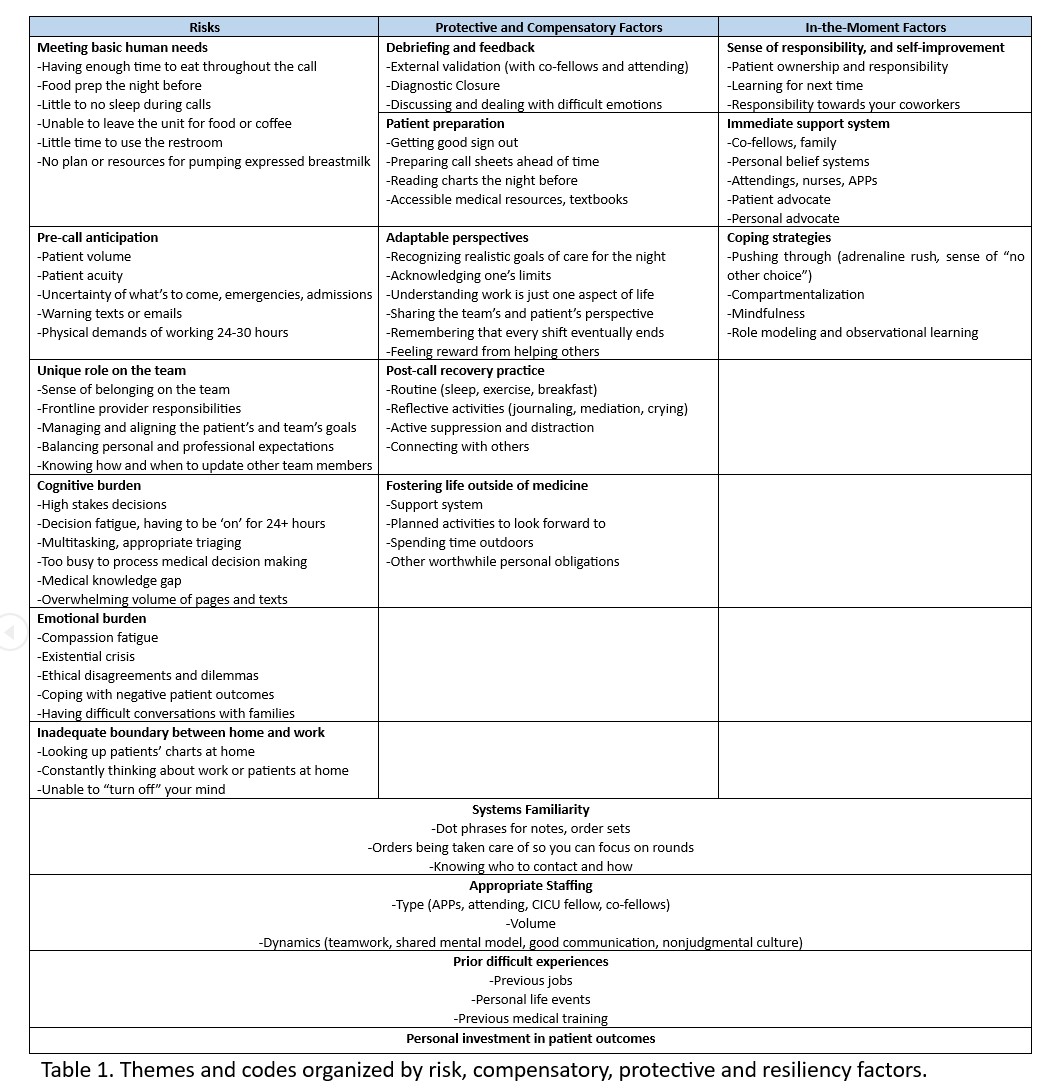
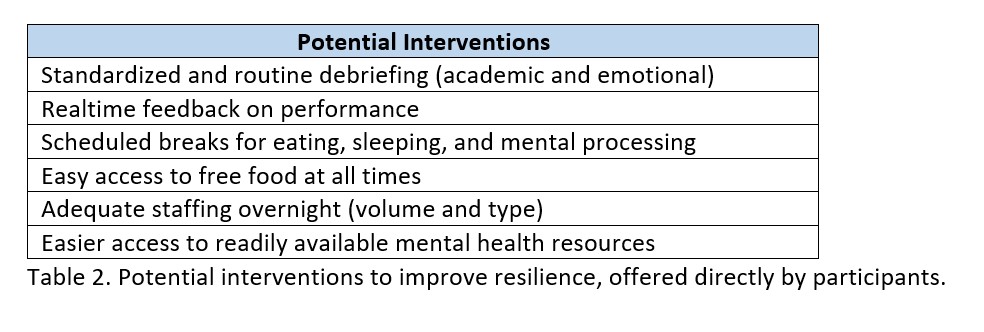
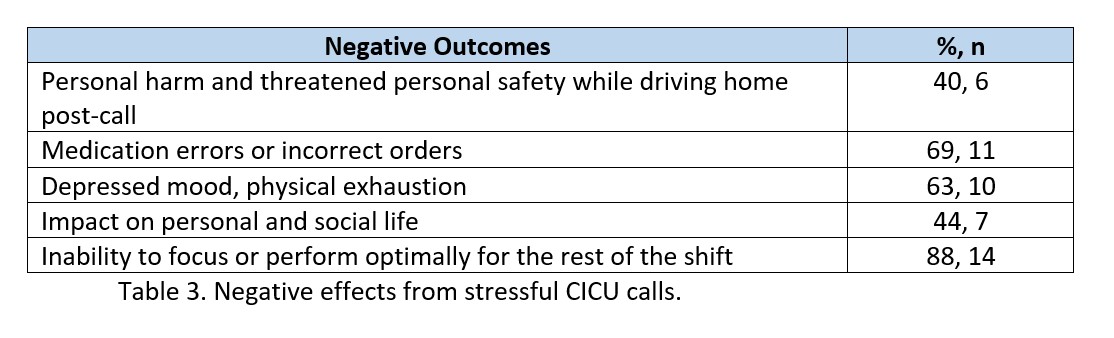
Results: Baseline demographics showed that 87.5% of the participants met the primary definition of burnout. Analysis from 16 total participants show the following predominant themes for risk factors for stress in the CICU: meeting basic human needs, pre-call anticipation, inability to separate work and home, and cognitive and emotional burden. Some of the main themes for protective and compensatory factors for resilience were debriefing and feedback, adaptable perspectives, and post-call recovery practices. Finally, ‘in-the-moment’ factors were explained through a sense of responsibility and self-improvement, immediate support system, and coping strategies. We found that systems familiarity and appropriate staffing spanned all three major categories. See the attached table for all themes and codes. Potential interventions offered by the participants themselves included real-time feedback and debriefs, easier access to mental health resources, and scheduled breaks. Negative effects from call were reported as medication errors and incorrect orders (69%), personal harm while driving home post-call (40%), and the inability to focus or perform optimally after stressful shifts (88%).
Conclusion(s):
Through this study, we have identified specific factors and potential interventions on the personal, programmatic, and institutional level that could improve fellowship training and physician resilience, and may minimize patient and personal harm.