Emergency Medicine: All Areas
Emergency Medicine 10
460 - Discontinuing Antibiotics for Pediatric Emergency Department Patients with Contaminant Urine Cultures
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 460
Publication Number: 460.309
Publication Number: 460.309
Yvette Wang, Rady Children's Hospital San Diego, San Diego, CA, United States; Tatyana G. Mills, University of California, San Diego School of Medicine, San Diego, CA, United States; Elise Zimmerman, Rady Children's Hospital San Diego, San Diego, CA, United States; Begem Lee, University of California, San Diego School of Medicine, San Diego, CA, United States; Patricia Soto, Rady Children's Hospital San Diego, Chula Vista, CA, United States; Simon J.. Lucio, University of California, San Diego School of Medicine, San Diego, CA, United States; Amy W. Bryl, University of California, San Diego School of Medicine, San Diego, CA, United States
- YW
Yvette Wang, MD
Assistant Clinical Professor of Pediatrics
Rady Children's Hospital San Diego
San Diego, California, United States
Presenting Author(s)
Background: In the pediatric emergency department (PED), patients diagnosed with urinary tract infections (UTIs) are started on antibiotics based on urinalysis results while awaiting urine cultures (UCx). If UCx are not consistent with UTIs, antibiotics can be safely discontinued. Previously at our institution, pediatric emergency medicine (PEM) physicians reviewed culture results daily, but patients with UCx growing contaminants were not contacted and continued antibiotics unnecessarily.
Objective: For patients diagnosed with presumed UTIs but found to have contaminant UCx, our aim was to increase the percentage of patients who had antibiotics discontinued from 4% to 75% by May 31, 2022.
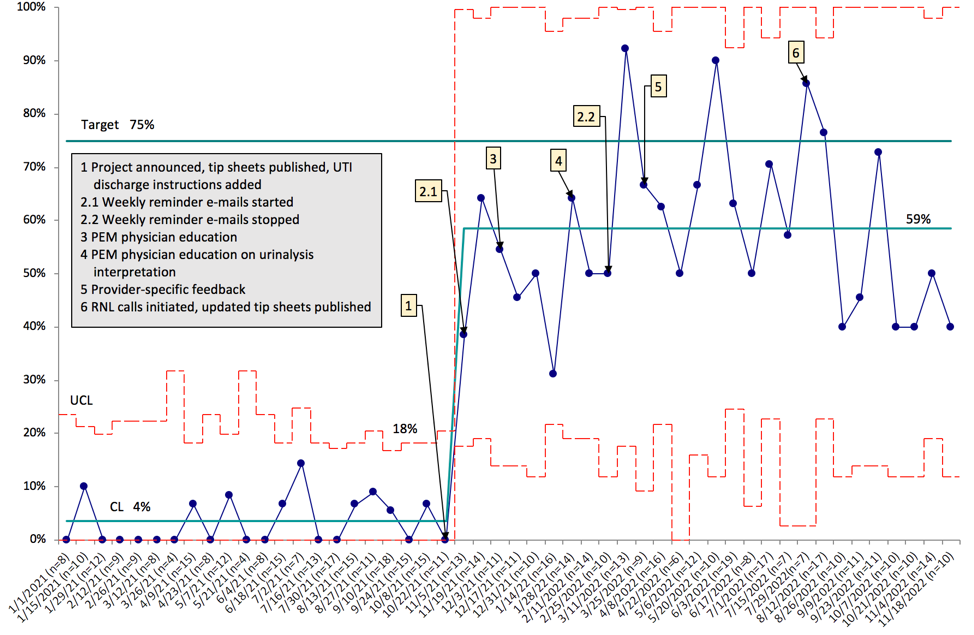
Design/Methods: Our multidisciplinary team created a key driver diagram to determine areas of intervention (Figure 1). Plan-Do-Study-Act cycle interventions focused on PEM physician education and feedback, patient education, and enhancing efficiency in managing UCx. We later trained resource nurse line (RNL) staff to contact families regarding contaminant UCx results and created a new workflow to send results to RNL staff. Outcome measures were the proportion of patients with contaminant UCx who had antibiotics discontinued and the average antibiotic duration for patients with contaminant UCx. Process measures were the proportion of patients called by PEM physicians and RNL staff. Balancing measures were the proportion of patients with antibiotics discontinued who returned to the PED within 7 days with urinary symptoms and the estimated additional time per day spent by PEM physicians on UCx calls. We used statistical process control to examine changes in measures over time.
Results: The proportion of patients who had antibiotics discontinued by PEM physicians and RNL staff increased from 4% to 59% within 6 months, sustained for an additional 6 months (Figure 2). The average antibiotic duration for patients with contaminant UCx decreased from 7 (UCL 8, LCL 6) to 5 (UCL 7, LCL 3) days. The proportion of patients called by PEM physicians and RNL staff increased from 6% (UCL 25%, LCL 0%) to 80% (UCL 100%, LCL 43%). Of the patients who had antibiotics discontinued, 3 returned with urinary symptoms. We estimated that before engaging the RNL, PEM physicians spent an additional 3 (UCL 5, LCL 1) minutes daily calling these patients.
Conclusion(s): We increased the proportion of patients with contaminant UCx who had antibiotics discontinued by 55% and ensured sustainability by implementing a new process with RNL staff making these phone calls.
.png)