Hypertension
Hypertension 1
7 - Baseline Cardiovascular Health in Youth Referred for Hypertension Disorders across U.S. Geographic Regions: a SUPERHERO Interim Analysis
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 7
Publication Number: 7.321
Publication Number: 7.321
Estefania G. Narvaez, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Waxhaw, NC, United States; Kiri W.. Bagley, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Shupti Biswas, Cohen Children's Medical Center, Floral Park, NY, United States; Aaron M. Bridges, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Wilkesboro, NC, United States; Lucy D'Agostino McGowan, Wake Forest University, Winston Salem, NC, United States; Victoria Giammattei, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, winston-Salem, NC, United States; Margret Kamel, Emory University School of Medicine, Atlanta, GA, United States; Stefan G. Kiessling, Kentucky Children's Hospital, Lexington, KY, United States; Jackson T. Londeree, Emory, Atlanta, GA, United States; Caroline B. Lucas, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Jason Misurac, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Margaret Murphy, University of Kentucky College of Medicine, Lexington, KY, United States; Sandeep Riar, Emory University School of Medicine, Atlanta, GA, United States; Christine Sethna, Cohen Children’s Medical Center, New Hyde Park, NY, United States; Irina Viviano, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Donald J. Weaver, Levine Children's Hospital, Charlotte, NC, United States; Andrew M.. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States

Estefania G. Narvaez (she/her/hers)
Undergraduate Student
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Waxhaw, North Carolina, United States
Presenting Author(s)
Background: Youth experiencing health disparities may face substantial barriers relating to the social determinants of health (SDOH), including geographic isolation. Patients residing in isolated geographic areas often face lengthy travel distances to obtain care, with accompanying financial and cultural burdens. These health risks can lead to complications in youth with hypertension. However, it is unknown how cardiovascular health varies across the U.S. in youth with hypertension.
Objective: Describe the geographic differences in baseline cardiovascular health in youth referred for hypertension disorders.
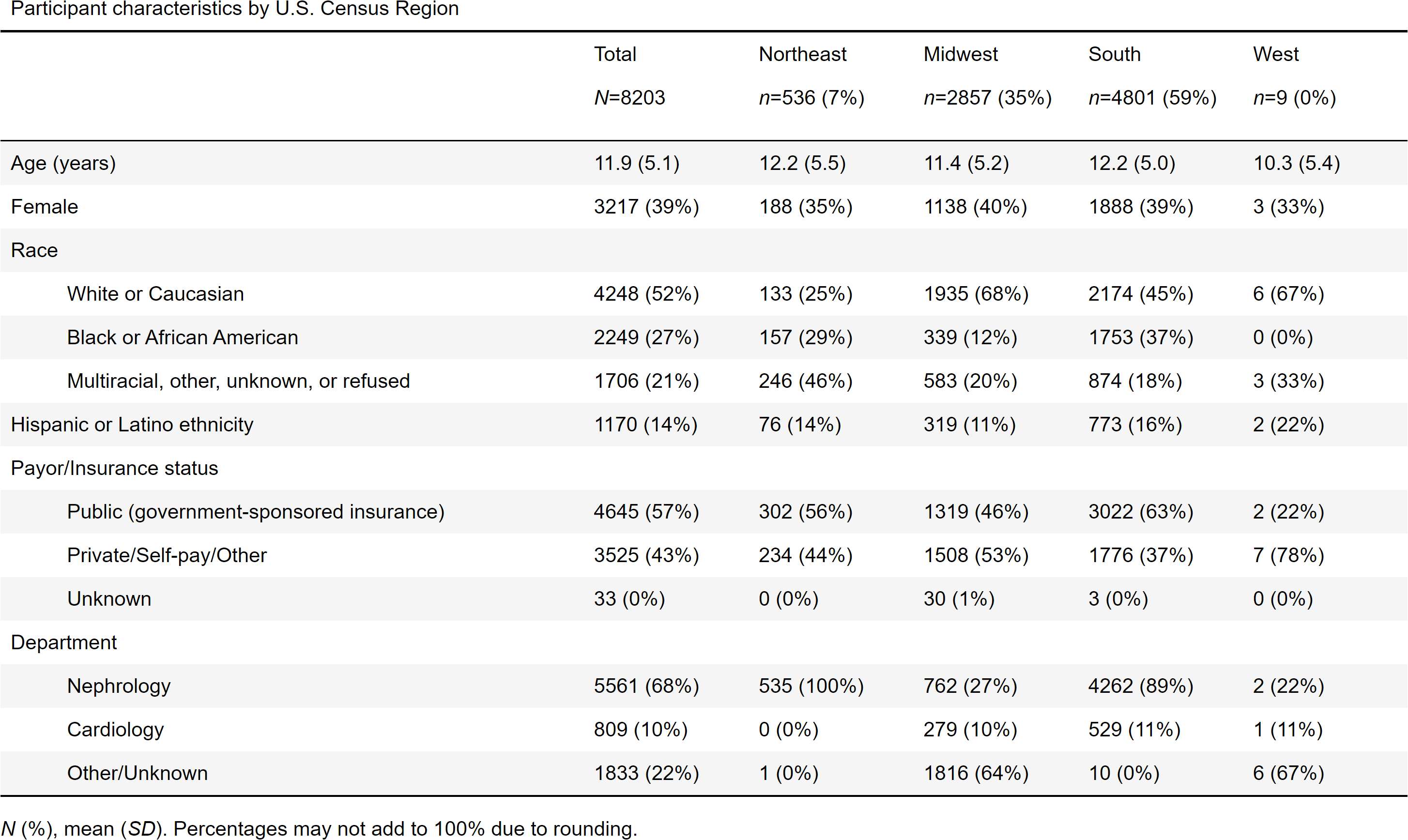
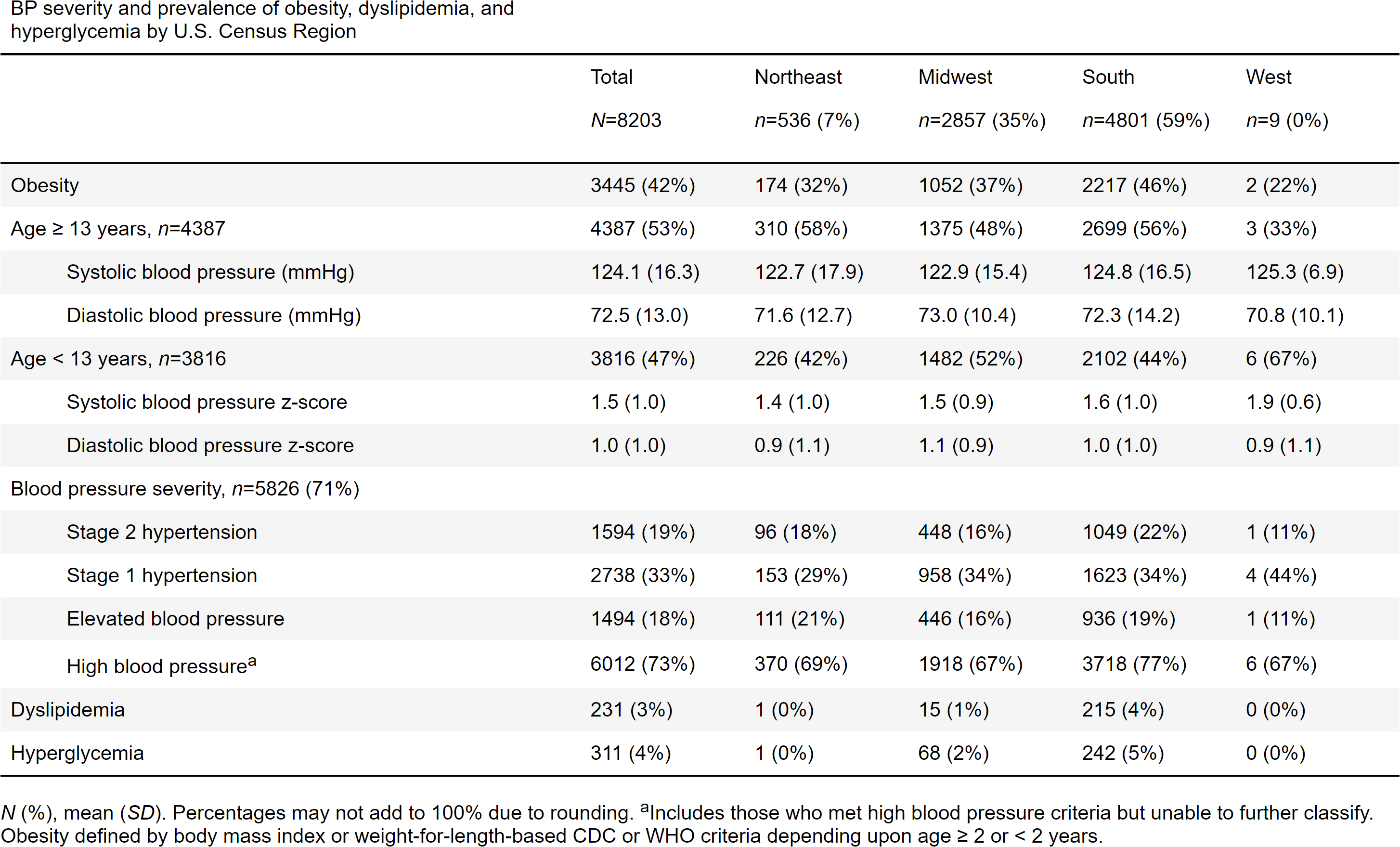
Design/Methods: Interim analysis of baseline data from The Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multisite retrospective cohort using data from the electronic health record. Inclusion criteria were initial visit for hypertension disorder (identified by ICD-10 code) between 1/1/2015 and 12/31/2021 and age < 19 years. Exclusion criteria were ICD-10 code-identified kidney failure on dialysis, kidney transplant, or pregnancy at the initial visit. We recorded U.S. Census geographic Region based on participants’ home addresses. Our outcomes were blood pressure, body mass index (age ≥2 yr.) or weight-for-length (age < 2 yr.) percentile-defined obesity, and ICD-10 code-defined dyslipidemia or hyperglycemia. We used chi-square test or Fisher exact test to compare outcomes across levels of the exposures.
Results: Of the 8,203 participants, mean age was 11.9 years (SD 5.1), 39% were female, 52% were White or Caucasian, 27% were Black or African American, and 14% were Hispanic or Latino (Table 1). Regional distribution included 59% in the South, 35% in the Midwest, 7% in the Northeast, and 0.1% in the West. The South had the highest p</span>roportion of blood pressure severity and had substantially higher prevalence of obesity (46%), dyslipidemia (4%), and hyperglycemia (5%) (Table 2). The Northeast had the least severe blood pressure and a lower prevalence of obesity.
Conclusion(s): We observed statistically significant differences between geographic areas in the U.S. and cardiovascular health at the index clinic visit in youth referred for hypertension disorders. Specifically, the South region had worse cardiovascular health overall. Understanding implications of SDOH for the health and well-being of children in geographically remote areas can help inform approaches tailored to their specific needs, barriers to care, and areas of opportunity.