Cardiology
Cardiology 2
756 - Neurodevelopmental outcomes among children with congenital heart disease born prematurely
Publication Number: 756.304
.jpg)
Jenna A. Katz, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Boston Children's Hospital
Newton Centre, Massachusetts, United States
Presenting Author(s)
Background:
Congenital heart disease (CHD) and prematurity are the leading causes of death in the first year of life in the United States. Infants with CHD have a 2-to-3-fold greater risk of premature birth compared to those without CHD. These infants are often described as facing “double jeopardy,” with vulnerability from their underlying heart disease and from organ immaturity. Premature infants with CHD are known to have higher morbidity and mortality, but less is known about long-term neurodevelopment in this population.
Objective: To investigate the association of gestational age (GA) with neurodevelopmental outcomes among children with CHD who underwent cardiac surgery in infancy.
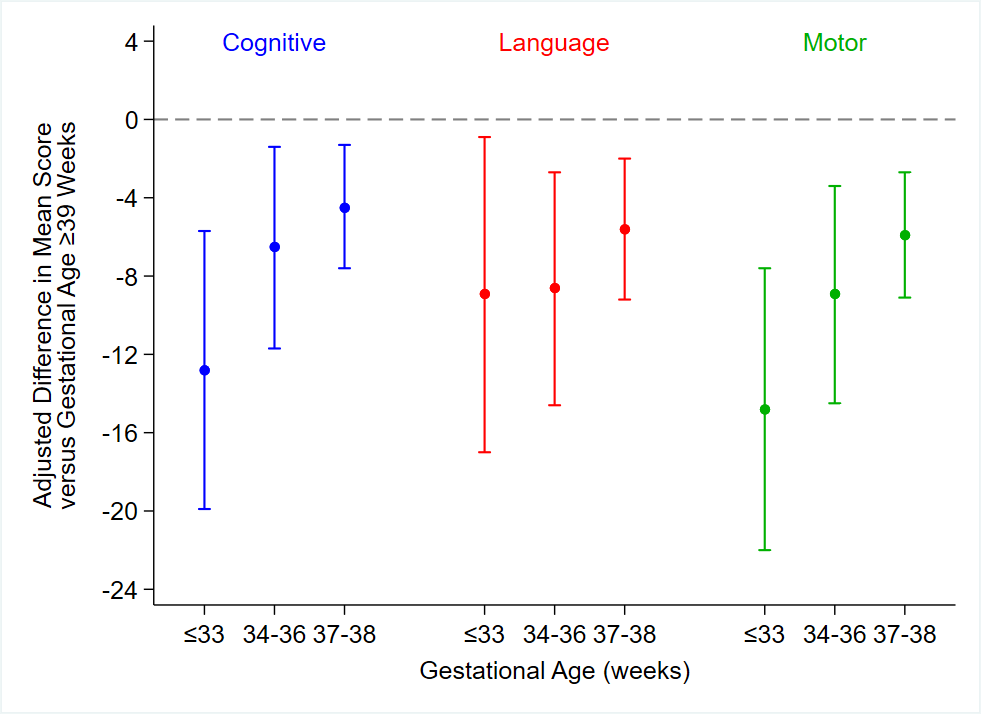
Design/Methods: We performed a single-institution retrospective study from 2007 to 2020 of all children who underwent cardiac surgery in the 1st year of life and a developmental evaluation between 12-30 months of age with the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III). Patients were stratified into 4 groups based on GA: very/moderately preterm (< 34 weeks), late-preterm (34 to < 37 weeks), early-term (37 to < 39 weeks) or term/post-term (≥39 weeks). Bayley-III outcomes were compared across GA groups using multivariable linear regression adjusting for primary caregiver level of education, sex, single ventricle anatomy, genetic abnormalities, and extracardiac abnormalities.
Results:
Cardiac surgery was performed in 1359 infants during the study period. Of those, 453 (33%) had a developmental evaluation, including a Bayley-III, after discharge; 18 were preterm, 37 late-preterm, 114 early-term, and 284 term/post-term. Patients who did versus did not return for developmental follow-up were similar in their demographic factors and GA. In univariate analyses, mean Bayley-III cognitive and motor domain composite scores were higher with greater gestational age. On the language domain, premature infants as a group had the lowest composite scores, but the late preterm group scored somewhat lower than the very/moderately preterm group. When adjusting for preoperative risk factors, composite scores were higher across all three domains as gestational age increased, with the preterm, late-preterm, and early-term groups scoring statistically significantly lower than the term/post-term group (Figure).
Conclusion(s): Gestational age is a strong independent risk factor for adverse neurodevelopmental outcomes in infants with CHD. Further multi-disciplinary research should explore whether optimized timing of delivery or index cardiac surgery, enhanced developmental care, and/or other interventions can mitigate this risk.