Critical Care
Critical Care 3
769 - Nutrition support adequacy in critically ill children admitted to neuro ICU
Publication Number: 769.306

Marwa Mansour, MD
Pediatrics critical care Fellow
critical care Medicine Fellowship- Texas Children's Hospital, Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Studies report challenges in achieving adequate nutrition intake in the first days of admission to the PICU and that delayed achievement of macronutrient targets beyond 7 days in the PICU is associated with greater mortality.
Objective: The study aims to evaluate nutrition support adequacy in critically ill patients in neuro ICU.
Design/Methods:
Retrospective cohort study of children admitted (index) to Neuro ICU with medical and surgical primary diagnosis from 01-19 to 12-19. We included patients with ICU LOS >7 days who received enteral and/or parental nutrition. Underweight assessed by WHO and CDC weight for age charts (WFA z score < -2). Caloric and protein adequacy defined as (Intake/BMR by Schofield equation) and (Intake/1.5 g/kg as recommended by ASPEN 2017). Optimal adequacy defined as (intake/prescribed ≥ 60%). Analyses by unpaired t-test and Chi-Square.
Results:
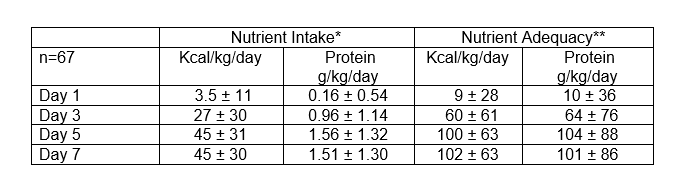
Of 515 pts, 67 patients were enrolled (42% females). Three patients were on enteral keto diet. 15 patients were on TPN, with or without enteral feeds. The median (IQR) for age was 4.9 (0.79-11) yrs., weight 16.6 (8.5-35) kg, mechanical ventilation (MV) duration (n= 65) 189 (139-359) hours, PIM3 risk of mortality (ROM) 1.9 (0.78-4) %, ICU Length of stay (LOS) 13.4 (10-24) days, hospital LOS 27 (17-43) days. The prevalence of underweight was 20.9% and mortality was 5.9%. Diagnostic categories included: seizures (33%), infections (26%), neurovascular (17%), brain (12%), spinal cord (4.5%), Neuromuscular (3%), complications (3%), and anomalies (1.5%). The optimal caloric and protein adequacy prevalence at Days 1, 3, 5, and 7 was 7.5%, 51%, 79%, and 79%; and 7.5%, 43%, 70%, and 76%, respectively. By day 3 of admission, caloric adequacy was achieved by 68% of patients < 2 years old (n=25) and 40% patients >2 yrs old (n=42), p=0.03 and protein adequacy was achieved by 64% of patients < 2 yrs vs 30% of patients >2 yrs; p=0.008. Underweight patients (n=14) achieved caloric adequacy at 110±61 % vs 46±53% by non-underweight (n=53); p=0.0002 and protein 132±92% vs 46±60% adequacy by day 3, respectively; p< 0.0001. No statistical difference between macronutrient intake adequacy between medical (n=63) and surgical (n=4) patients was observed in this cohort.
Conclusion(s):
Optimal caloric and protein adequacy were reached by the majority of the patients by day 5 of admission. Younger patients < 2 years old reached faster adequate macronutrient adequacy compared to older patients. Underweight patients were more likely to achieve optimal adequacy compared to patients with normal nutritional status.