Critical Care
Critical Care 3
773 - The Impact of Secondary Stressors on Family Experience in the Pediatric ICU
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 773
Publication Number: 773.306
Publication Number: 773.306
Iris Chan, Tufts University School of Medicine, BOSTON, MA, United States; Annie J. Wang, Tufts Children's Hospital, Boston Children's Hospital, Boston, MA, United States; Robert Ohman, Seattle Children's Hospital/University of Washington, Seattle, WA, United States; Lisa DelSignore, Tufts Children's Hospital / Boston Children's Hospital, Boston, MA, United States

Iris Chan, BA (she/her/hers)
Medical Student
Tufts University School of Medicine
BOSTON, Massachusetts, United States
Presenting Author(s)
Background: A child’s hospitalization in the pediatric intensive care unit (PICU) is emotionally stressful for parents and may exacerbate existing stressors such as family and socioeconomic needs. No prior research has assessed the association between secondary stressors and amount of time parents spend with their hospitalized child. It remains unclear how stress perception varies between parents of different races/ethnicities.
Objective: Our primary aim was to evaluate the relation between secondary stressors and parents’ ability to be physically present during a child’s PICU admission. Secondary aims were to characterize the self-perception of secondary stressors and how these may vary with race/ethnicity.
Design/Methods: We conducted a prospective cross-sectional study over five months. Parents of hospitalized children in a 10-bed academic PICU completed a questionnaire rating perception of secondary stressors. Composite Stress Scores based on 10 secondary stressor groups (e.g. finances, food insecurity, transportation, childcare, family medical needs, PICU environment) were analyzed via chi-square to examine the relationship between parental stressors and hospital presence. Paired t-tests analyzed racial/ethnic differences in secondary stressors.
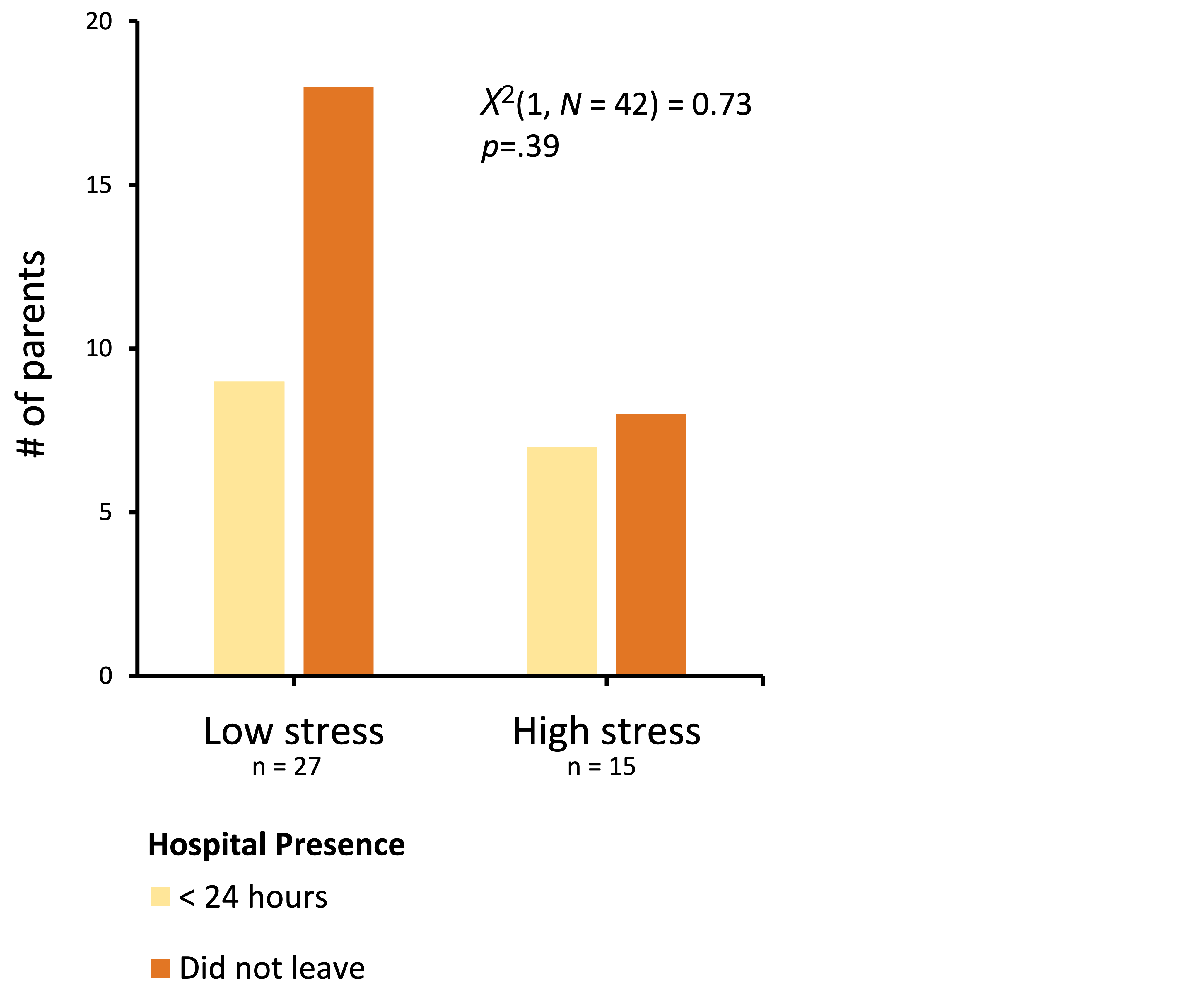
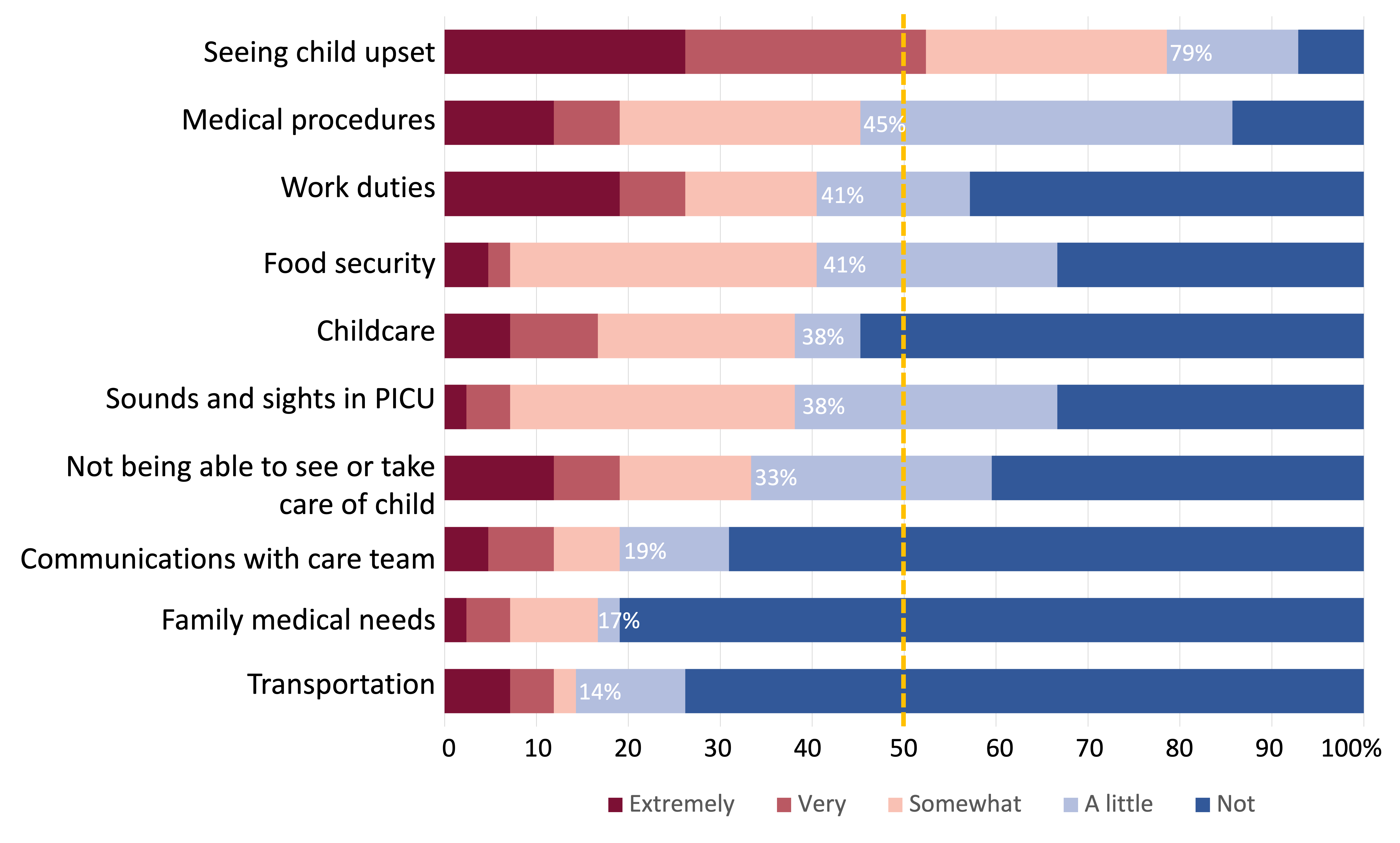
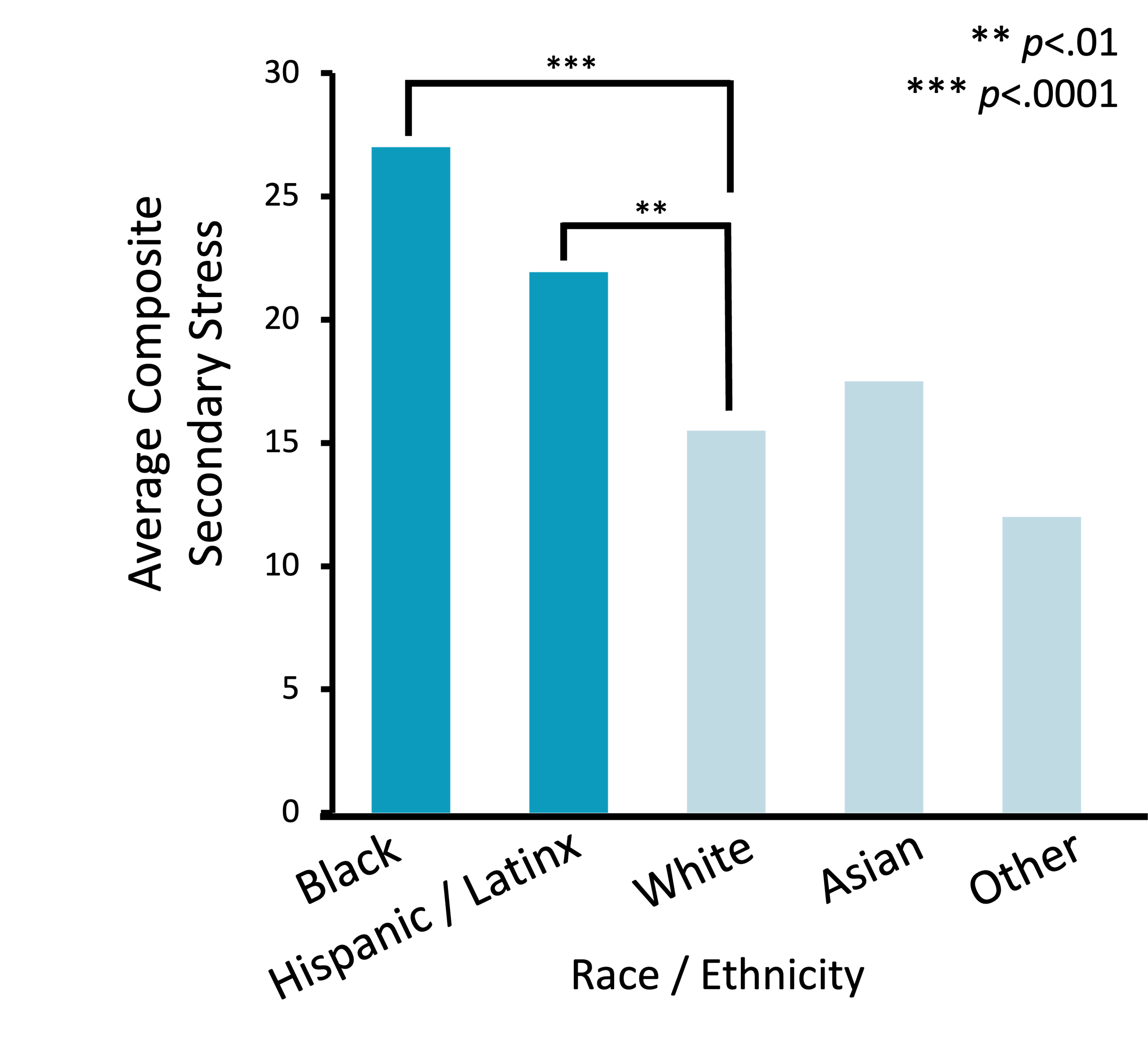
Results: Forty-two parents responded (85.7% response rate). Secondary stressors were not significantly associated with time physically spent in the PICU (p=.39, Fig.1). Sixty percent of parents did not leave the hospital. Of parents who left, 75% were present for more than 16 hrs/day. Parents perceived multiple stressors that were “somewhat, very, or extremely stressful” while their child was hospitalized (Fig. 2), including socioeconomic factors related to work duties (41%), food security (41%), and childcare (38%). Hispanic and Black parents experienced significantly higher stress compared to non-Hispanic White parents (p< .01, p< .0001, Fig. 3).
Conclusion(s): Self-perceived secondary stressors did not correlate with parents’ physical presence in the PICU. Racial disparities in self-perceived stress exist; Hispanic and Black parents reported higher secondary stressors during PICU hospitalization. Different drivers may moderate why parents with reported low and high secondary stress do not leave the PICU. These findings suggest that implementing an adapted PICU-specific survey may improve identification of patient populations at risk for high stress during hospitalization. More data are needed to better characterize systemic drivers of stress in underrepresented minorities during PICU hospitalization in order to develop targeted interventions to decrease this burden.