Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 7
679 - Using a health disparities framework to identify determinants of asthma morbidity among young children with asthma: A qualitative study
Publication Number: 679.318

Jordan Tyris, MD, MSHS (she/her/hers)
Pediatric Hospital Medicine Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Children < 5 years have rates of asthma-related morbidity that supersede all other pediatric age groups. Geospatial analysis has helped elucidate population-level associations between social determinants of health (SDOH) and these inequities, yet these analyses are not augmented with stakeholder-engaged qualitative data. This is necessary, as SDOH are entwined, and it is difficult to prioritize on which determinants interventions should focus.
Objective:
To characterize caregiver perceived determinants contributing to asthma morbidity among children < 5 years.
Design/Methods:
In this qualitative study, semi-structured interviews were conducted with caregivers of children < 5 years old and living in DC during their hospitalization for asthma. The interview guide was created using the Asthma and Allergy Foundation of America’s (AAFA) health disparities framework which includes 5 categories of determinants: structural determinants, social determinants, healthcare services, individual behaviors, and genes/biology (Figure 1). The AAFA, World Health Organization, and Healthy People SDOH frameworks informed a predetermined codebook of specific determinants. Interviews were analyzed with directed content analysis. Themes were mapped to specific determinants and organized according to the AAFA categories. Study rigor and triangulation were optimized with two methods. First, caregiver addresses were geocoded and linked to census tract Child Opportunity Index (COI), a composite measure of 29 place-based SDOH organized into three domains (Educational, Health/Environmental, Social/Economic). Second, pediatric providers from an asthma specialty clinic that provides enhanced care coordination addressing social factors were interviewed using the same guide.
Results:
Preliminary results included 1 provider and 7 caregivers. 100% of caregivers lived in census tracts with low/very low overall COI [Table 1]. Eight themes highlighting how determinants impact asthma morbidity have been identified, mapping to 6 determinants and all 5 AAFA categories (Table 2). The most frequently reported themes focused on health literacy, children’s individual behaviors, and quality of housing/environmental conditions. Two additional themes highlighted how conversely, asthma morbidity impacts determinants. These included socioeconomic position (ability to attend school/work) and psychosocial factors (stress).
Conclusion(s):
In this qualitative study with ongoing recruitment, caregivers perceive that determinants both impact, and are impacted by, asthma morbidity among children < 5 years. 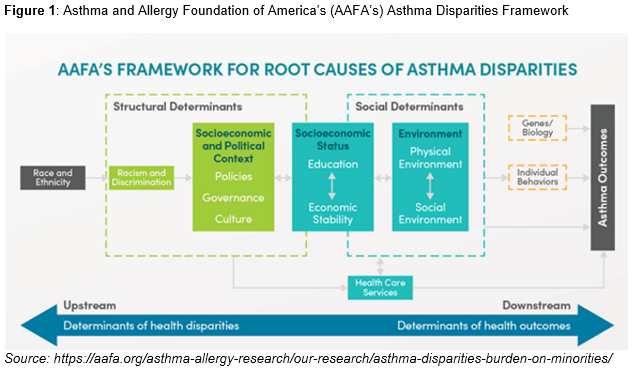
.png)
.png)
