Medical Education: Medical Student
Medical Education 12: Student 2
567 - Investing in Medical Student Learning by Supporting Belonging in Clinical Settings
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 567
Publication Number: 567.326
Publication Number: 567.326
Amy Creel, LSUHSC, New Orleans, LA, United States; Terry Kind, Children's National Hospital / George Washington University, Washington, DC, United States; Nikita Nagpal, New York University Long Island School of Medicine, New York, NY, United States; Chris Peltier, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Joseph A. Jackson, Duke University School of Medicine, Durham, NC, United States; Amal Khidir, Weill Cornell Medicine in Qatar, Doha, Ar Rayyan, Qatar; Caroline Paul, NYU Grossman School of Medicine, New York Cigy, NY, United States; Gary L. Beck Dallaghan, University of Texas at Tyler School of Medicine, Tyler, TX, United States; Chad Vercio, Loma Linda University School of Medicine, Redlands, CA, United States; Helen C. Wang, University of California, San Diego, La Jolla, CA, United States
- AC
Amy Creel, Md (she/her/hers)
Associate Professor of Pediatrics
LSUHSC
New Orleans, Louisiana, United States
Presenting Author(s)
Background: A shift in learning environments occurs when medical learners rotate in clinical settings. Patient care is integrated alongside, and at times compete with, education. Success in situational learning occurs when Maslow’s three needs for self-motivation are met. Team dynamics in clinical settings factor into sense of belonging (SB) and its role in ability and motivation to learn, however, the specific relationships and their impact on medical students have not been adequately explored. Increased understanding of factors that affect learning in clinical settings is needed to optimize learning environments. We explored characteristics of team based clinical medicine to inform and support development of intrinsically motivated lifelong learning for all medical students.
Objective: Explore medical students’ SB in clinical medicine in relation to learning.
Design/Methods: As part of a larger multi-institutional study exploring Professional identity formation, a group of pediatric educators used a phenomenological approach to explore the contributions of SB to learning in senior medical students in clinical settings. We conducted one hour Zoom focus groups from 2/2022-5/2022. Prompted written reflections and self reported demographics were collected after each session using an anonymous online tool. Investigators worked in teams using an iterative process to inductively code verbatim transcriptions.
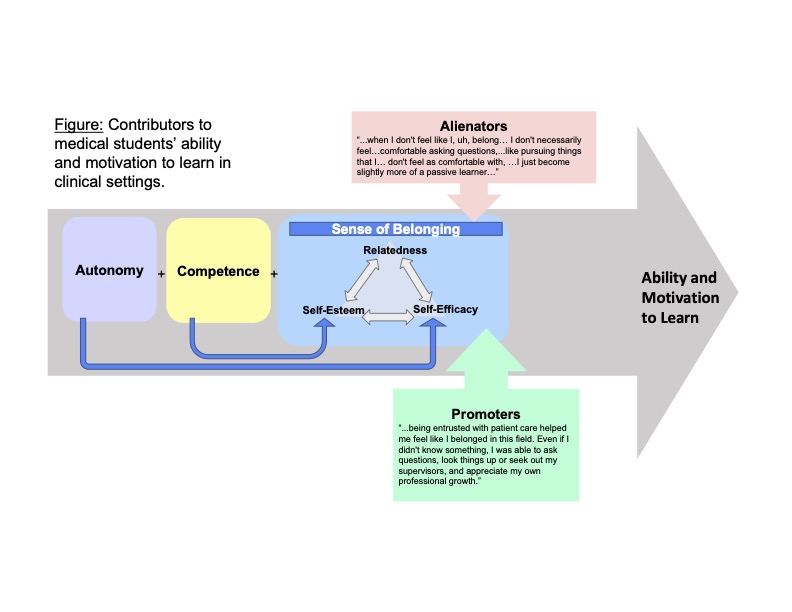
Results: Twenty-six senior medical students participated from six United States medical schools. Participants shared that increased SB in clinical medicine positively affected their ability and motivation to learn. Specifically, increased SB on the clinical rotation was associated with comfort in: asking questions, answering knowledge questions, attempting procedures, and presenting patient care plans. Conversely, learning was impacted negatively by contributors to alienation including: feeling like a liability, being ignored or unseen, strict adherence to hierarchy, lack of active participation, inadequate feedback, and the evaluation and grading process. See Figure.
Conclusion(s): Senior medical students on clinical rotations report experiences with SB to have a profound effect on their ability and motivation to learn. Our findings are consistent with self-determination theory and reaffirm that autonomy and competency impact students’ intrinsic motivation to learn. Intentional strategies to improve SB and avoid alienation for medical students are needed to support learning. Possible strategies include: providing autonomy support, ensuring psychological safety, and enhancing relational closeness.