Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 3
400 - Diagnostic Utility of Tracheal Aspirate Cultures in the NICU
Publication Number: 400.334
Madeline M. Keane (she/her/hers)
Medical Student
Burnett School of Medicine at Texas Christian University
Fort Worth, Texas, United States
Presenting Author(s)
Background:
Tracheal Aspirate cultures (TA) are routinely drawn from intubated NICU patients in the diagnostic workup for infection due to CDC criteria for CLABSI. Clinicians must often differentiate TA results in the clinical context of colonization vs infection. Antibiotic stewardship improves neonatal outcomes.
Objective:
Describe the tracheal microbiome of intubated patients in the NICU.
Determine the diagnostic validity of TA in intubated NICU patients.
Design/Methods:
All TAs were prospectively monitored from a Level IV NICU over an 11-month period beginning February 2022. Positive cultures were used to describe the observed tracheal microbiome of intubated NICU patients. Among positive TAs, we determined a diagnosis of pneumonia, tracheitis, colonization, or contamination via real-time physician surveys and compared their diagnoses to an independent, retrospective chart review. Chart review diagnoses were based on published criteria for the diagnosis of pneumonia or tracheitis in the pediatric population.
Results:
117 TAs were sent from the NICU during the study epoch. Patient demographics are listed in Table 1.
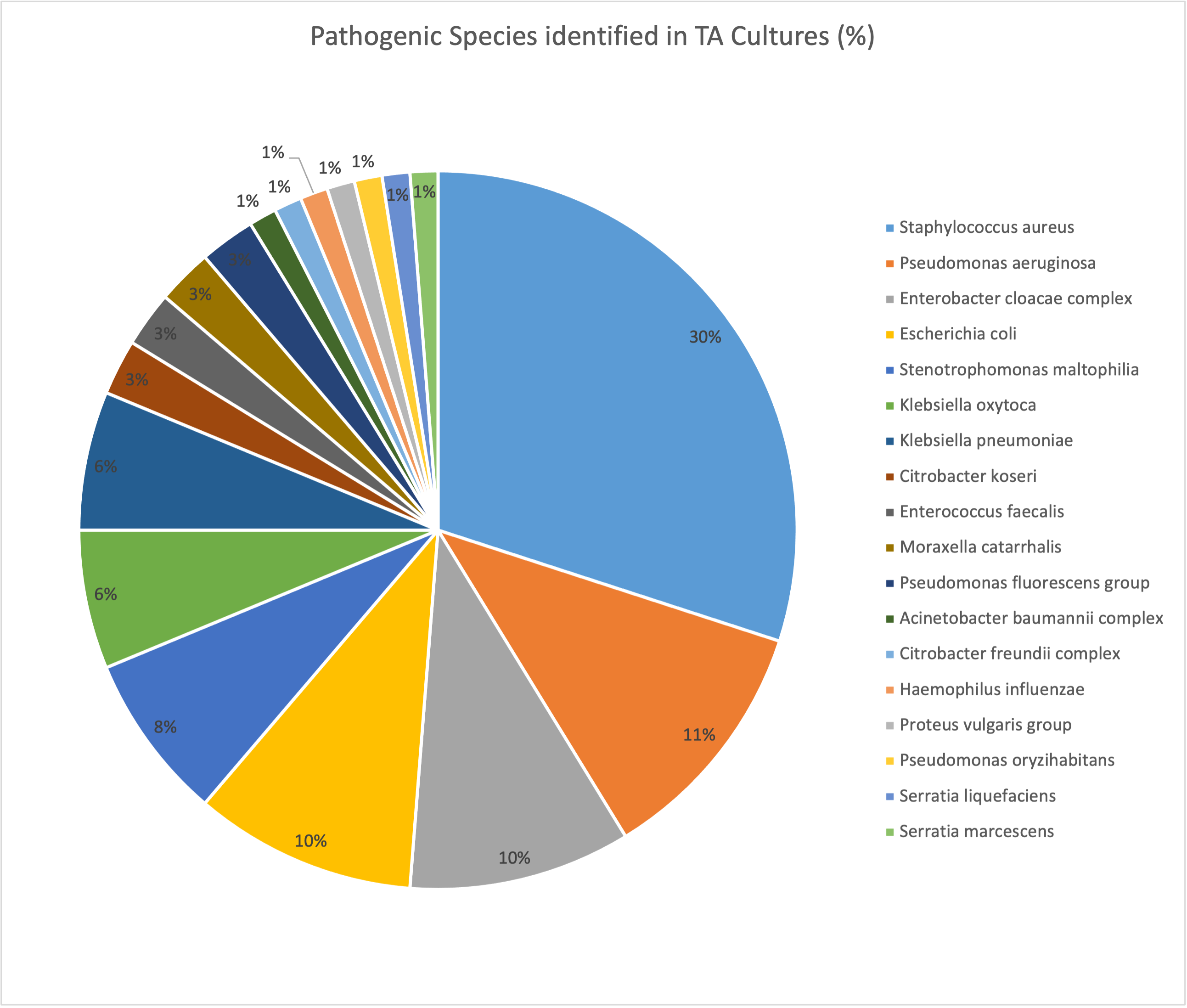
Pathogenic bacterial species grew in 55 cultures (47%), most commonly Staph aureus.
Oropharyngeal flora grew in 25 cultures (21%). Eleven infants (20%) simultaneously grew a pathogenic organism from blood, urine, or CSF. The distribution of pathogenic organisms in the tracheal microbiome is illustrated in Figure 1.
Among infants with pathogenic TA growth, 96% were treated with more than 2 days of antibiotics. Physician diagnoses of treated infants included pneumonia (36%), tracheitis (38%), and colonization (24%).
Chart review revealed 20/55 (36%) of the positive cultures did not meet established clinical criteria for infection.
Based on initial physician diagnosis, the utility of TA in this population had a specificity of 86% and a positive predictive value of 72%. The independently validated diagnostic utility was reduced to a specificity of 76% and a PPV of 64% (Table 2).
Conclusion(s):
The observed microbiome of intubated NICU patients includes a wide variety of pathogenic organisms. Positive TAs often occur in the absence of true infection.
Despite a common physician diagnosis of colonization, most infants still received a prolonged course of antibiotics when a pathogenic organism was identified from TA. Independent chart review reveals physicians overestimated the incidence of true infection, also leading to increased antibiotic use.
Developing and implementing a more rigorous set of clinical guidelines for the interpretation of TAs is an opportunity to improve antibiotic stewardship in the NICU..png)
.jpg)
