Hypertension
Hypertension 1
13 - Prevalence and risk factors of disordered eating behavior in youth with hypertension
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 13
Publication Number: 13.321
Publication Number: 13.321
Ella C. Perrin, Naval Medical Center San Diego, San Diego, CA, United States; Andrew M.. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Hanna Ravi, University of Colorado, Denver, CO, United States; Gagana S. Borra, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Canton, MI, United States
- EP
Ella C. Perrin, MD, BS (she/her/hers)
Resident
Naval Medical Center San Diego
San Diego, California, United States
Presenting Author(s)
Background: Eating disorders in adolescents are increasing in prevalence and have adverse health consequences, but remain underdiagnosed. Patients with medical conditions that require lifestyle management, such as obesity and diabetes mellitus, have higher disordered eating behavior (DEB) risk (20–39%) than the general adolescent population (10%). Patients with CKD might also be at increased DEB risk. In youth with other conditions requiring lifestyle counseling—such as HTN—DEB prevalence and associated risk factors are unknown.
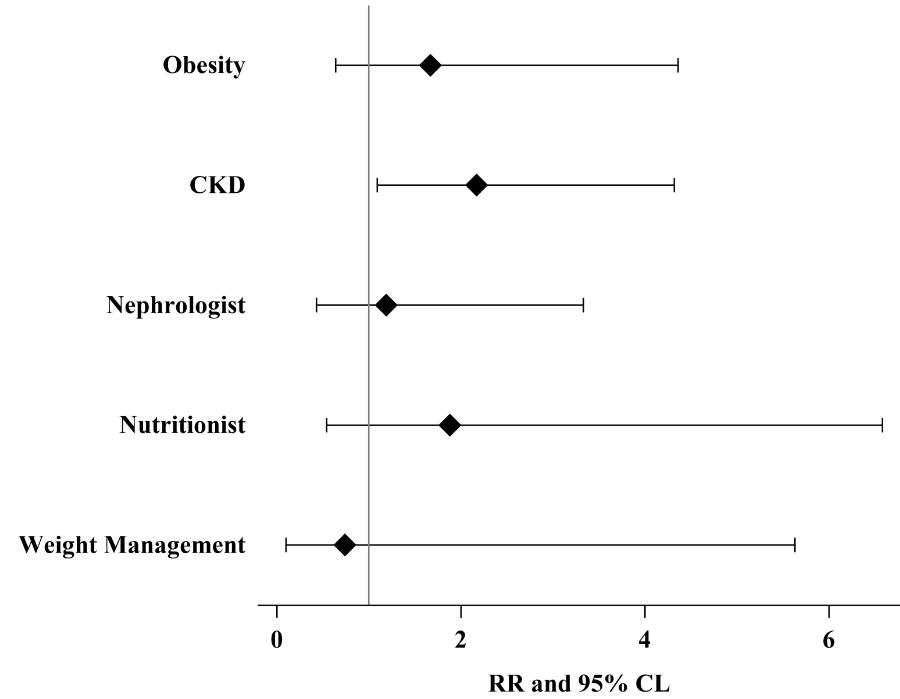
Objective: Estimate DEB prevalence in youth with HTN compared to the general adolescent population and investigate whether obesity, CKD, or less specialized lifestyle counseling source are associated with higher DEB risk.
Design/Methods: Prospective cross-sectional study of youth aged 11–18 years with HTN. We excluded patients with diabetes mellitus, kidney failure or transplantation, or gastrostomy tube dependence. We collected data via surveys and electronic health record abstraction. We administered the validated SCOFF DEB screening questionnaire wherein a score ≥2/5 is positive. We compared DEB prevalence using a one-sample z-test of proportions (p0=0.1) and estimated DEB risk by obesity, CKD, or lifestyle counseling using multivariable generalized linear models.
Results: Of 74 participants, 59% (44/74) identified as male gender, 22% (16/74) as Black or African American, and 36% (27/74) as Hispanic; 58% (43/74) had obesity and 26% (19/74) had CKD. DEB prevalence was 28% (95% CI 18–39%, p< 0.001). CKD was associated with higher DEB prevalence (adjusted RR 2.17, 95% CL 1.09 to 4.32), but obesity and lifestyle counseling source were not.
Conclusion(s): DEB prevalence is higher in youth with HTN and comparable to that reported in other conditions requiring lifestyle counseling. Concurrent CKD is associated with more than double the risk of DEB in this population. Youth with risk factors such as HTN and CKD may benefit from routine DEB screening.