Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 7
678 - Starting Somewhere – Piloting a Social Needs Screening & Community Resource Referral Project in a Pediatric Emergency Department with Help from an Undergraduate Research Program
Publication Number: 678.318

Natalie J. Tedford, MD (she/her/hers)
Pediatric Emergency Medicine & Global Health Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
Clinical research and screening programs can be time-intensive and challenging to conduct in busy pediatric emergency departments (PED); simultaneously, unmet social needs (USN) are common among patients/families seeking care in the PED. Limited data exists on the utility of embedded research programs in the PED to initiate social needs screening and community resource referral.
Objective:
To describe and evaluate the effectiveness of an undergraduate research program initiating social needs screening and community resource referral in a PED
Design/Methods:
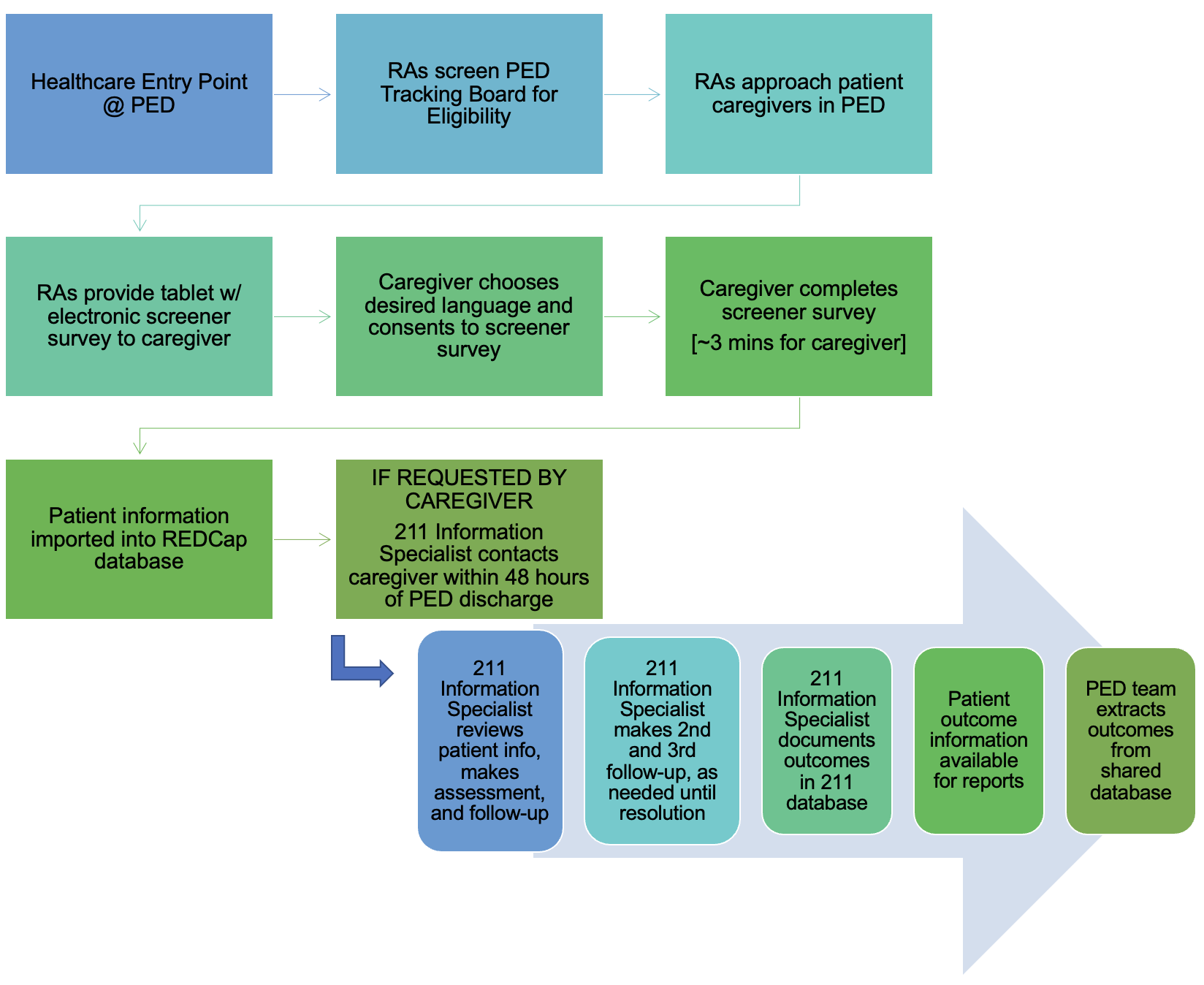
This was a cross-sectional study conducted in the PED at a quaternary level children’s hospital. Research assistants (RAs) utilized study workflow (Figure 1) to approach English- and Spanish-speaking caregivers of patients < 18 years old. Patients were excluded if >18 years old, legal caregiver not present, or other primary language. Caregivers were provided a tablet to self-enroll and completed social needs screening tool with the option to request community referral (211). Referral to 211 occurred within 48 hours of PED discharge. The primary outcome was screening rates of the PED census during RA-coverage with secondary outcomes including USN rate and 211 referral rates. Secondary analysis compared screening and referral rates from RA-based project to current social work(SW)/care management (CM) consults in the PED. Data were analyzed using descriptive statistics.
Results:
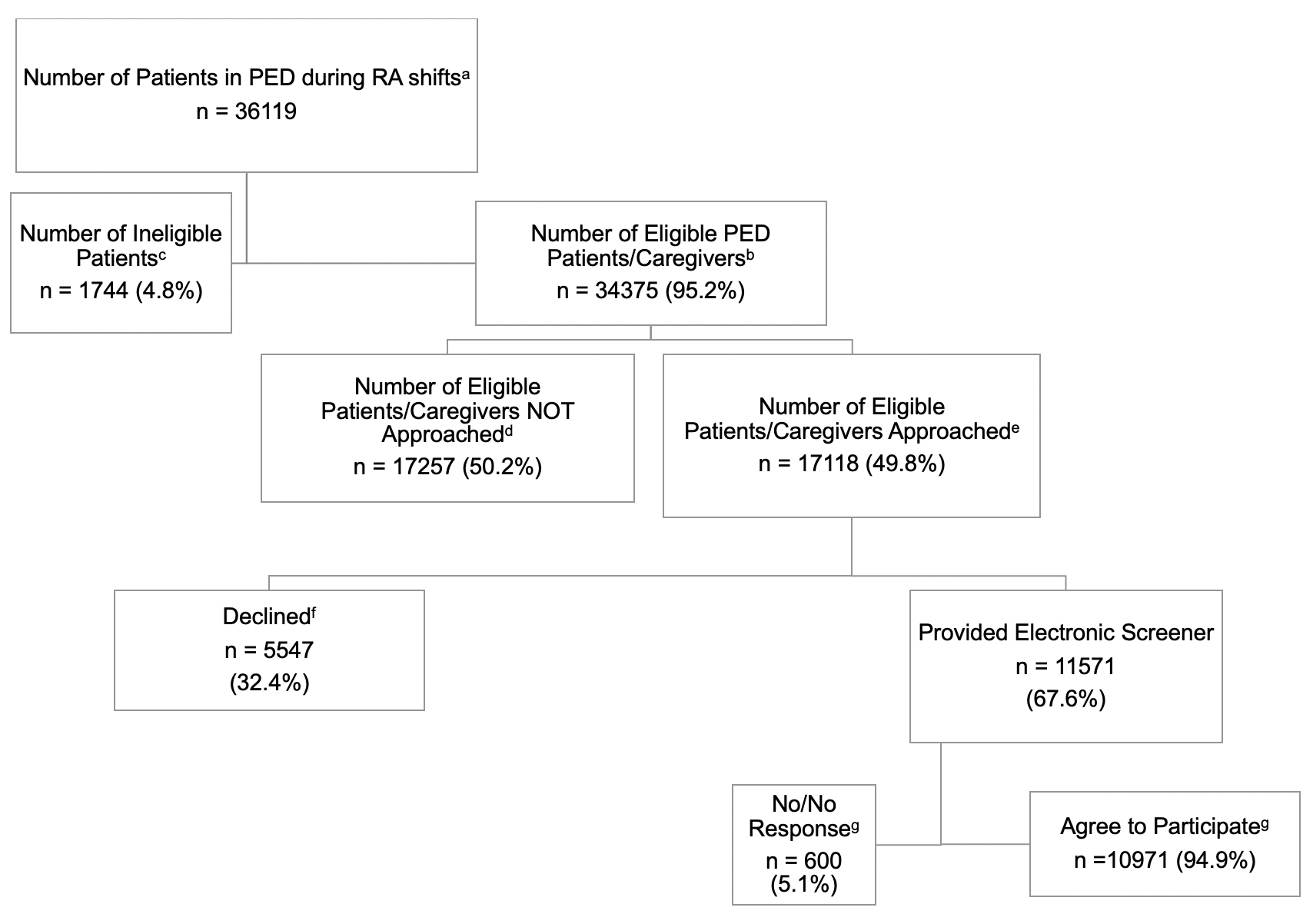
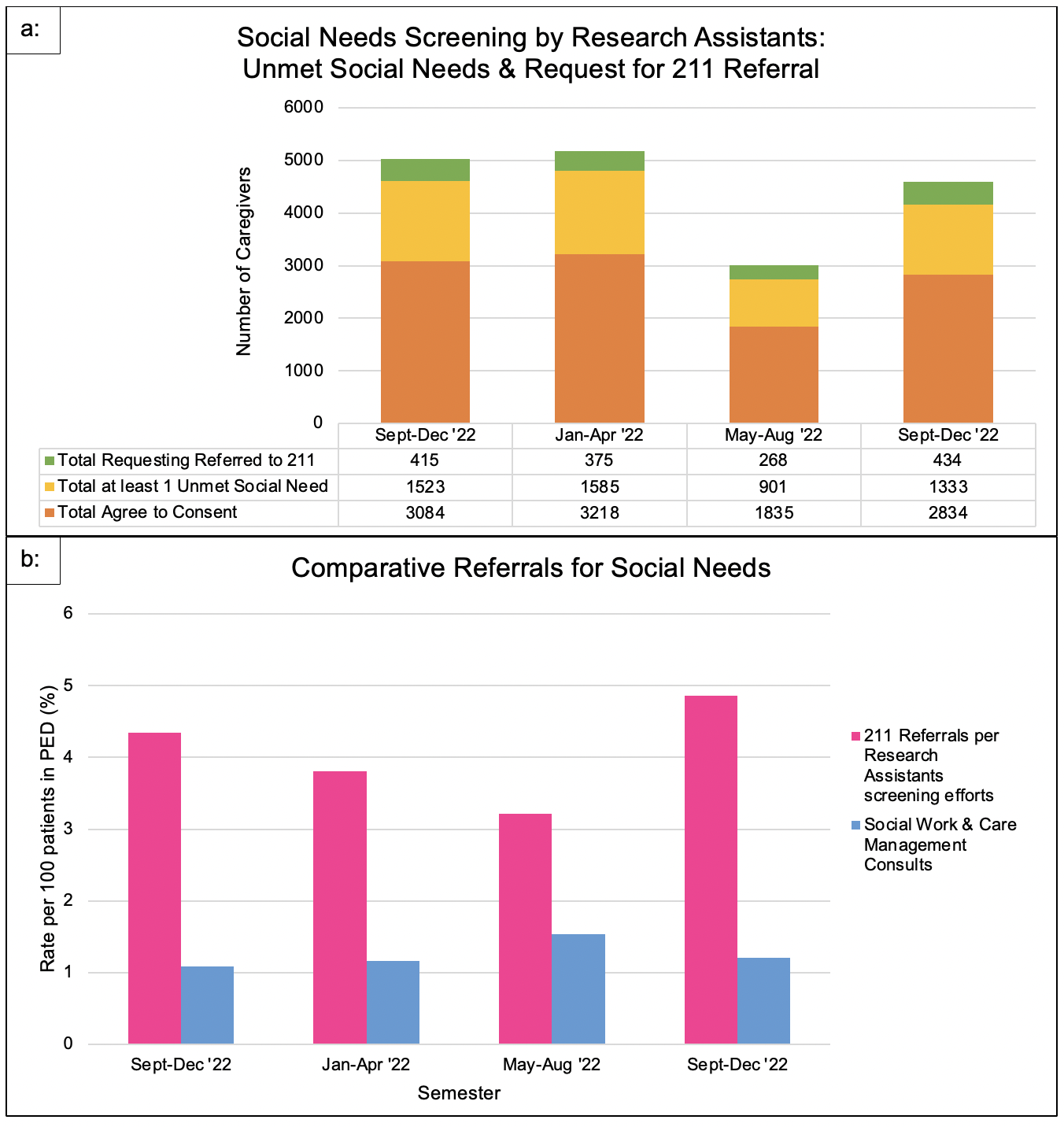
From 09/27/21 to 12/7/22, 36119 presented to the PED during RA-coverage with 34375 eligible (95.2%), 17118 approached by RAs (49.8%), and 11571 caregivers provided electronic screener (33.6%) (Figure 2). Of the caregivers given the electronic screener, 10971 consented to participate (95%). Of those participating, 5342 reported ≥1 USN (48.7%) and 1492 requesting 211 referral (13.9%) (Figure 3a). Semester screening rates over the 4 semesters had a mean of 32.1% (23.8-40.2%) of PED census. Screening with requested referral rates from RA-based project compared to SW/CM consults demonstrated the RA-based project resulted in 2 to 4 times more referrals to community resource referral (Figure 3b).
Conclusion(s):
The use of an undergraduate research program can enhance social needs screening and referral practices during PED visits and initiate upstream efforts to address social determinants of health within a healthcare system. This study also highlights how RAs and community partnerships can aid in offloading hospital teams. Next steps include implementing sustainable screening practices in the PED workflow and provide more immediate resources while awaiting community referral.