Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 1
215 - Failure of Head Growth, but not Weight, is Associated with hsPDA Exposure Among Preterm Infants Born at Less than 27 Weeks Gestation
Publication Number: 215.329

Krista Bergquist-Stumme (she/her/hers)
Medical Student
University of Iowa Roy J. and Lucille A. Carver College of Medicine
Iowa City, Iowa, United States
Presenting Author(s)
Background:
Persistent hemodynamically significant patent ductus arteriosus (hsPDA) following preterm birth results in circulatory disturbance whereby pre-ductal [e.g. brain, heart] circulation is hyperperfused and post-ductal [e.g. enteric] circulation may be hypo-perfused which may impact growth. hsPDA has been associated with impaired neurodevelopment and literature suggests that both somatic growth and brain volume may be adversely affected; however, these studies typically used aggressive fluid restriction and diuretics.
Objective:
To characterize the association between hsPDA exposure beyond the transitional period ( >3 days) and postnatal head circumference (HC) and somatic growth at 6 weeks postmenstrual age.
Design/Methods:
A cohort study of neonates born < 27 weeks’ gestation, admitted between 11/18-06/21, was conducted. Enrolled patients had standardized echocardiography at < 24h postnatal age, day 5-7 and regularly thereafter until resolution of hsPDA. By clinical practice, hsPDA therapy does not include routine use of diuretics or fluid restriction. Patients with anasarca, genetic/major anomalies were excluded. Patients were classified as hsPDA-exposed patients if the Iowa PDA score [Table 1] was ≥6 during the study period and treatment for PDA was received. Duration and magnitude [mean PDA Score*days exposed] of hsPDA exposure were evaluated. A composite primary outcome of death before 42 days [longest shunt duration] or growth failure [weight±HC for age loss >-0.8 z-score] at 42±3 days. Univariate analysis and logistic regression were performed.
Results:
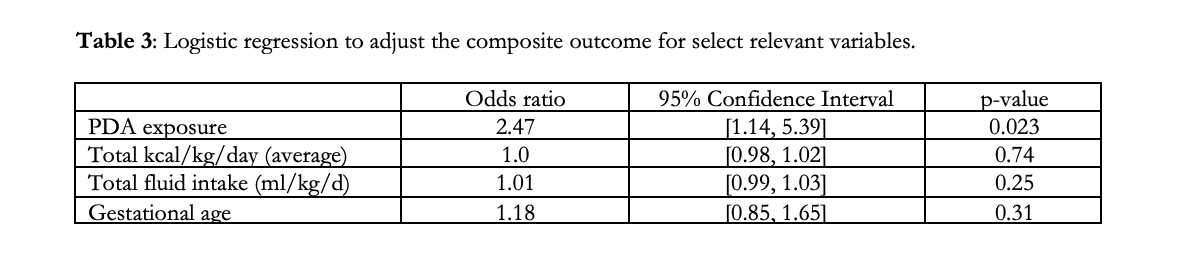
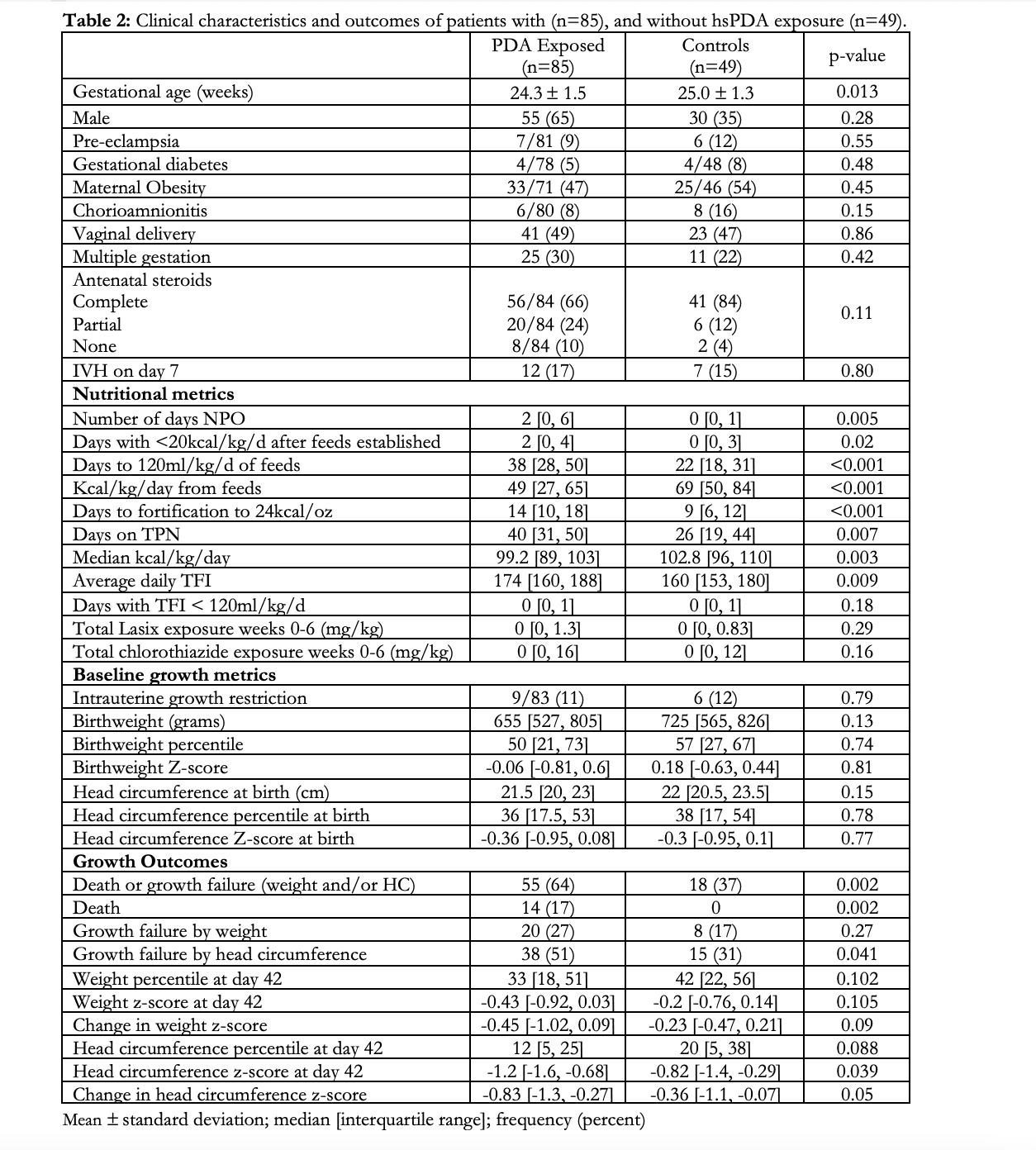
A total of 134/150 eligible patients were included. hsPDA-exposed (n=85) infants had a 3-fold higher risk of the composite outcome compared to controls. [Table 2] Failure of HC, but not somatic growth was more likely in hsPDA exposed patients; specifically, both HC z-score and change in HC z-score were lower. Median PDA duration [20.5 (6.3, 28) vs 13 (3, 28), p=0.14] and median cumulative PDA score [137 (48, 181) vs. 96 (10, 176), p=0.1] were higher among patients with HC growth failure. Exposed infants received less enteral feeds and less total calories, but more intravenous fluid. Logistic regression, to adjust the risk of composite outcome for nutritional exposure, fluids and gestational age (GA), revealed an OR of 2.54 for PDA exposure. [Table 3]
Conclusion(s):
Extremely preterm neonates exposed to hsPDA beyond the transitional period have a greater risk of death and failure of HC, but not somatic growth, independent of gestational age at birth and early nutrition. Further studies into catch-up growth and nutritional modifiers merit consideration.
.png)