Mental Health
Mental Health 3
716 - Pediatric Clinician Perspectives on Suicide Screening: Worries, Time and a Willingness To Learn New Things
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 716
Publication Number: 716.328
Publication Number: 716.328
Edan S. Leshem, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Andrew E. Solsrud, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Sherry K. Dodd, University of Washington School of Medicine, Wildwood, MO, United States; Shannon Rook, Washington University in St. Louis School of Medicine, Marthasville, MO, United States; Lauren Ericson, Washington University in St. Louis School of Medicine, Saint Louis, MO, United States; Ruoyun Wang, Washington University in St. Louis School of Medicine, Saint Louis, MO, United States; Sharon A. Graham, Washington University in St. Louis School of Medicine, Saint Louis, MO, United States; Katie Plax, Washington University in St. Louis School of Medicine, Saint Louis, MO, United States

Edan S. Leshem (he/him/his)
Clinical Coordinator
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Suicide prevalence in youth has increased since the beginning of the COVID-19 pandemic, and pediatric primary care providers (PCP) are unsure how to systematically assess suicide risk and complete safety planning.
Objective: This study aims to grasp PCPs’ perspectives and strategies on suicide screening, risk assessment and safety planning for patients given the new AAP recommendation to screen.
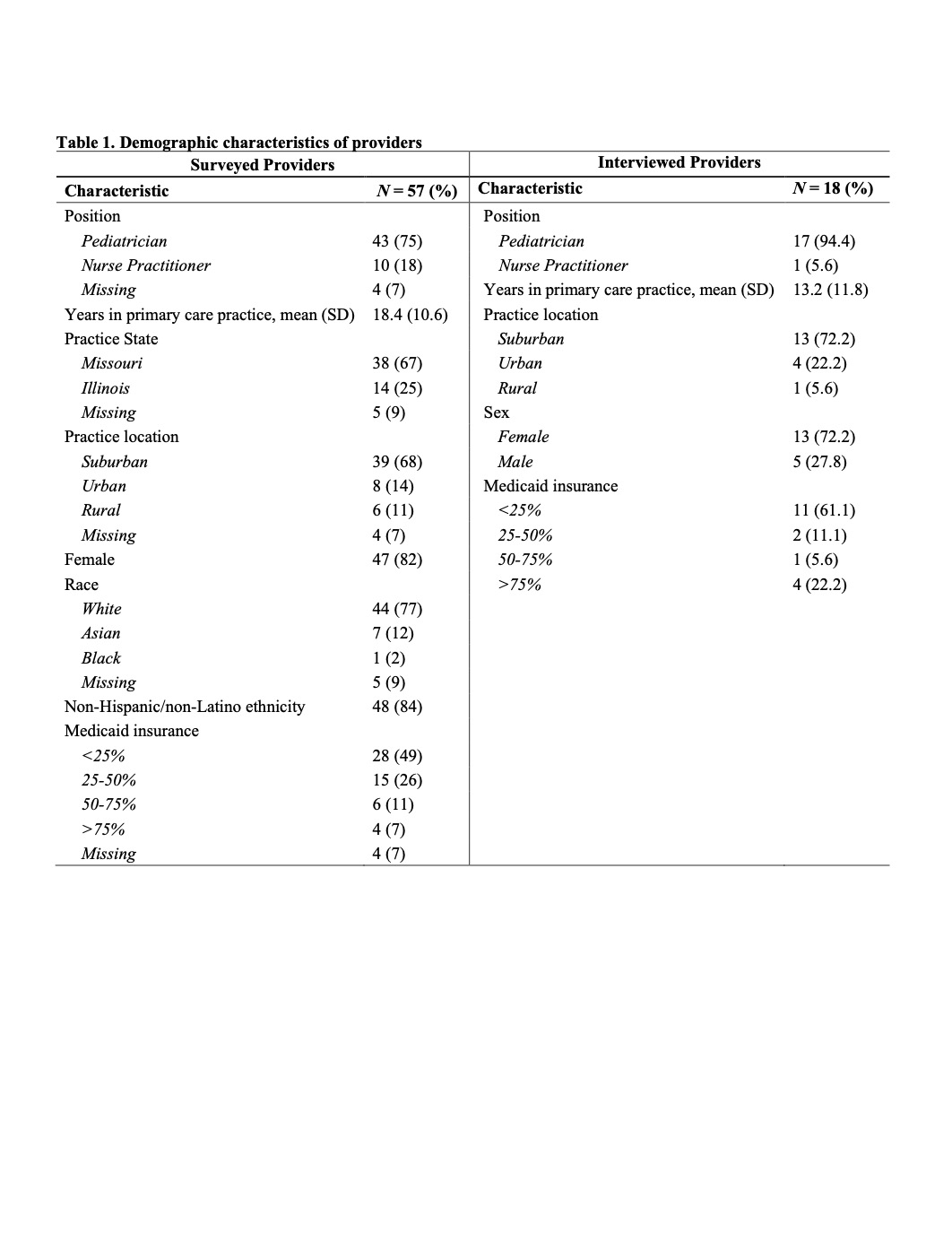
Design/Methods: Eligible participants were PCPs who provided mental health care for patients. Participants could participate in two ways: a 30-minute interview or a REDCap survey with invitations extended through a listserv in a local Pediatric PCP Learning Collaborative formed during the COVID-19 pandemic. 18 PCPs participated in a recorded interview; 57 completed a survey. Using a predefined guide, recorded interviews asked providers’ perspectives on mental health, suicide risk screening, and assessment. We analyzed transcribed interviews with consensual inductive coding techniques until data saturation.
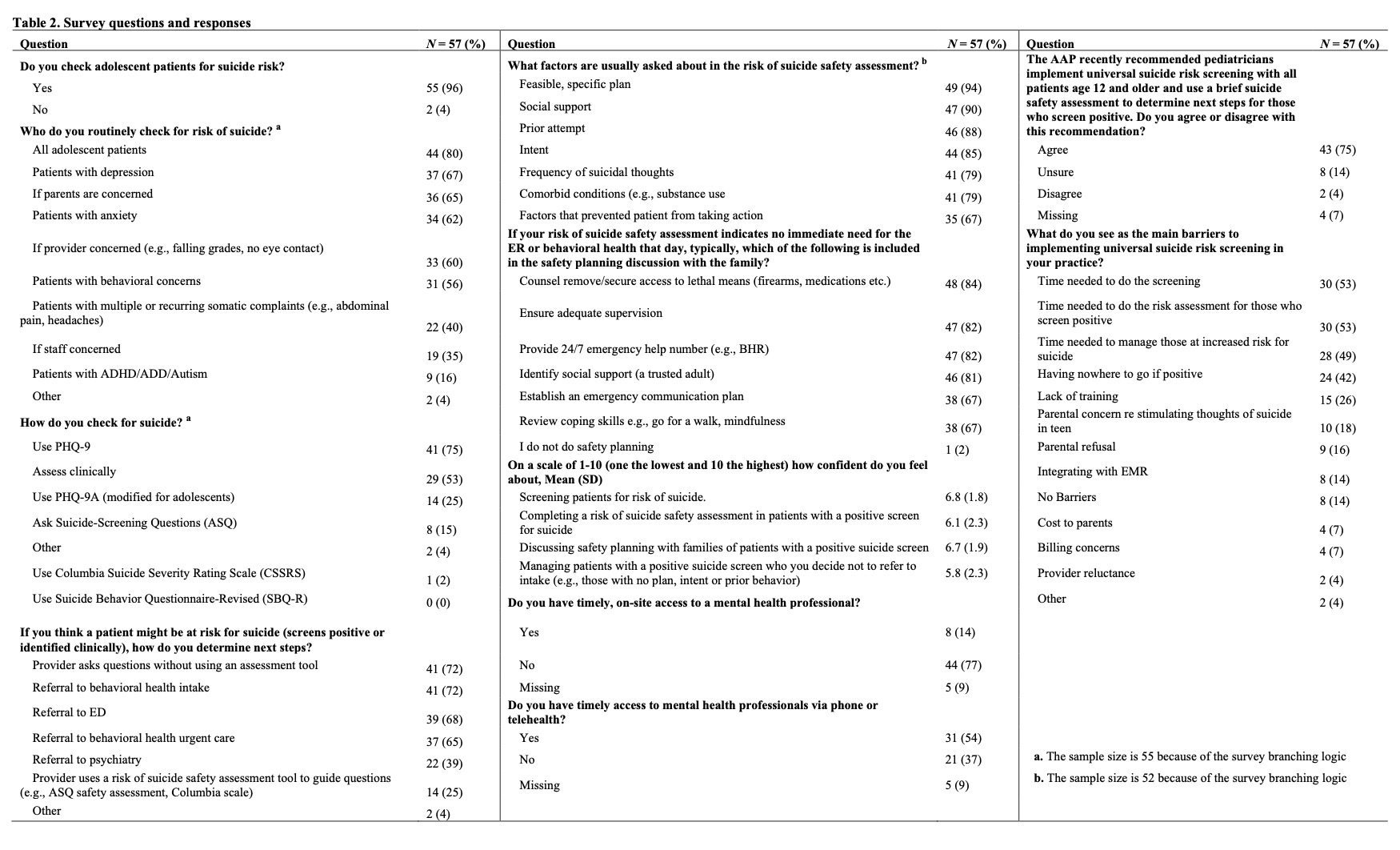
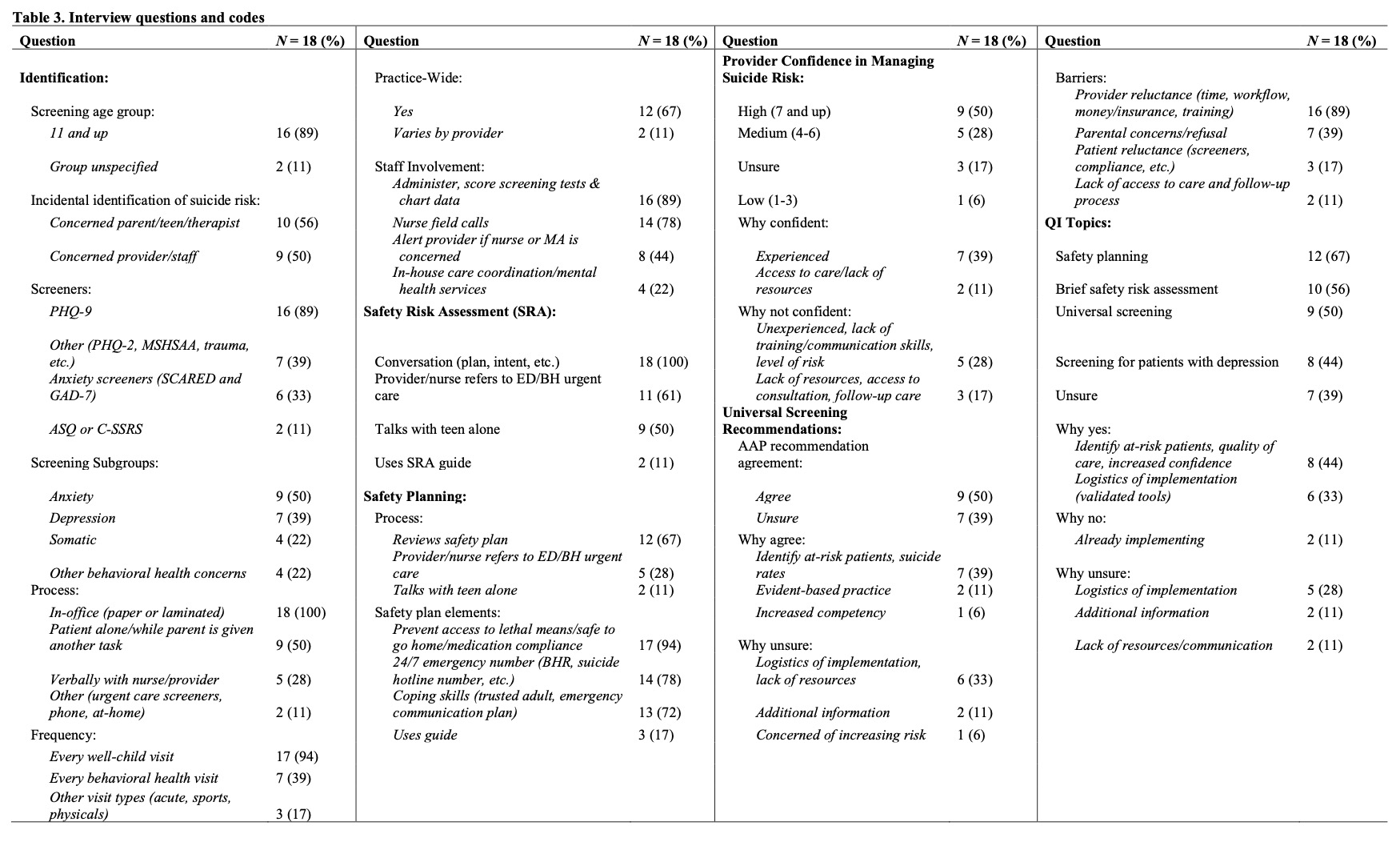
Results: Among the 57 PCPs that completed the surveys, 75% agreed with the new AAP universal screening recommendations and identified barriers for implementation in practice; time for screening (53%), time to assess those who screen positive (53%), time to manage those at increased risk (49%), lack of options for those who screen positive (42%), and lack of training (26%). Although most PCPs used the PHQ-9/9A to universally screen for both depression and suicide risk, only 16% of PCPs used a validated suicide screener. 93% of respondents were open to work on quality improvement (QI) projects.
18 interviewed PCPs employed strategies to identify suicide risk, few used suicide risk screeners (11%) and safety plan tools (11%). While PCPs indicated moderate confidence in managing patients with suicidal ideation, many were unsure how to best assess and address suicide risk due to lack of training (28%) or a lack of resources (17%). Half agreed with AAP screening recommendations but were concerned about implementation due to their own reluctance (89%) and parental concerns (39%). Overall, interviewed PCPs wanted to improve approaches to suicide prevention through QI projects focused on safety planning (67%), suicide risk assessment (56%), and universal screening (50%).
Conclusion(s): The findings suggest that PCPs need support and training to implement suicide screening, suicide risk assessment and safety planning. Timely, cost-effective strategies that do not obstruct workflow are priorities to increase PCP confidence in managing patients at risk for suicide.