Cardiology
Cardiology 2
760 - The Multimodality Assessment and Intramodality Comparison of Imaging Techniques in Relation to Pediatric Pulmonary Vein Stenosis
Publication Number: 760.304

Victor Kieu, MD
Fellow
Children's Hospital of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: Pulmonary vein stenosis (PVS) is a rare and progressive condition with a high mortality rate despite intervention (1). Evaluation usually involves multimodality imaging (2). Imaging generally includes transthoracic echocardiography (echo), computed tomography angiography (CTA) and lung perfusion scan (LP) with cardiac catheterization (cath) as the “gold” standard to provide the best assessment of PVS (3). There is unclear consensus on standardized criteria for PVS diagnosis (4,5,6), with limited comparisons between imaging modalities in pediatrics.
Objective: This study aimed to characterize how pulmonary vein assessment correlated across imaging modalities to help determine best practice diagnostic guidelines for characterizing pulmonary vein disease.
Design/Methods:
A single-center IRB approved retrospective pilot study at Children’s Wisconsin with documented PVS from 1/1/2004 to 6/1/2021 was completed. Subjects were excluded if all four imaging modalities were not done within a reasonable timeframe at diagnosis. Intramodality specific variables were compared between imaging methods with outcomes data obtained. Presence of absence of PVS was evaluated by Simple Kappa and/or Weighted Kappa coefficient between two modalities. Zero-weight observations were added for the missing categories to ensure a balanced contingency table. For intramodality specific variables, PVS was defined as >2mmHg by ECHO and Cath and/or reduction in diameter by CTA.
Results:
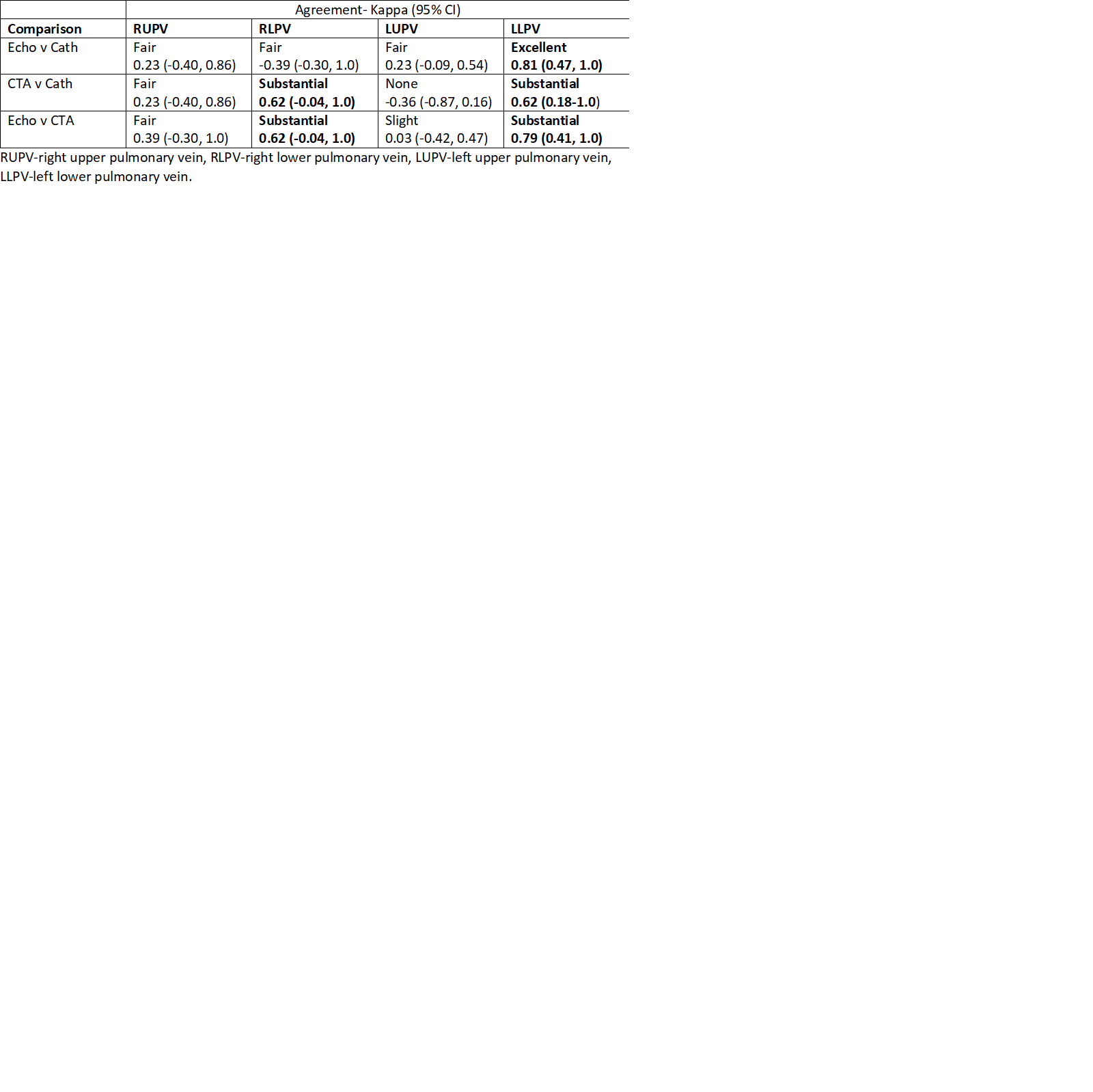
11 patients (7 males and 4 females) were identified. Median and (IQR) of gestational age was 27.0 (24.9, 34.0) weeks, and age at diagnosis was 237.0 (161, 329.0) days. The median (IQR) days from Cath to Echo were -11 (-27.0, -5.0), Cath to CTA were -4.0 (-18.0, 12.0), and Cath to LPS were 0 (-6.0, 2.0). There were a total of 20 stenosed pulmonary veins. CTA was better at identifying PVS in different vein locations than echo with the exception of the left upper pulmonary vein (LUPV) due to high false positive in CTA. CTA and echo did correlate with different vessels fairly well except with the LUPV. Table 1. Lung perfusion scan showed no agreement on affected vein sidedness compared to all other modalities since only most affected side had difference in perfusion.
Conclusion(s):
CTA appears to be the best non-invasive modality to characterize PVS location though with a significant false positive rate for LUPV. Future studies should correlate CTA and Cath with disease extent per vein and clinical outcomes to determine intervention suitability. (*References available upon request)