Medical Education: Simulation & Technology
Medical Education 9: Simulation & Technology 2
530 - Using Circumcision Simulation to Improve Pediatric Resident Knowledge and Comfortability
Publication Number: 530.327
- CF
Casey E. Freymiller, MD (he/him/his)
Research Fellow
Virginia Commonwealth University School of Medicine
Richmond, Virginia, United States
Presenting Author(s)
Background:
Knowledge of the circumcision process is an Accreditation Council for Graduate Medical Education (ACGME) requirement and pertinent to general pediatricians that manage patients in the post-op period. However, there is often limited exposure for pediatric residents with down-trending circumcision rates. Simulation models are documented in the literature but objective studies on the impact of simulation on learners are lacking.
Objective: This educational quality improvement project was begun to increase knowledge, comfortability, and desire to perform circumcisions with the use of a simulation model.
Design/Methods: All pediatric and medicine/pediatric residents at Virginia Commonwealth University were emailed an online survey to assess baseline competence and then given a lecture on the benefits, risks, contraindications, and necessary steps to perform a Gomco circumcision. Residents were then guided through the steps using appropriate instruments on a proprietary rubber model with glans, fascia, and skin layers. Afterwards, a post-simulation survey was sent. The following week, residents performed the procedure on the model without guidance while being evaluated by a proctor using a 20-point checklist. The primary outcome of the study was an increase in knowledge of the steps and comfortability performing after simulation. Secondary outcomes of the study were an increase in desire to perform a circumcision and checklist score after one week.
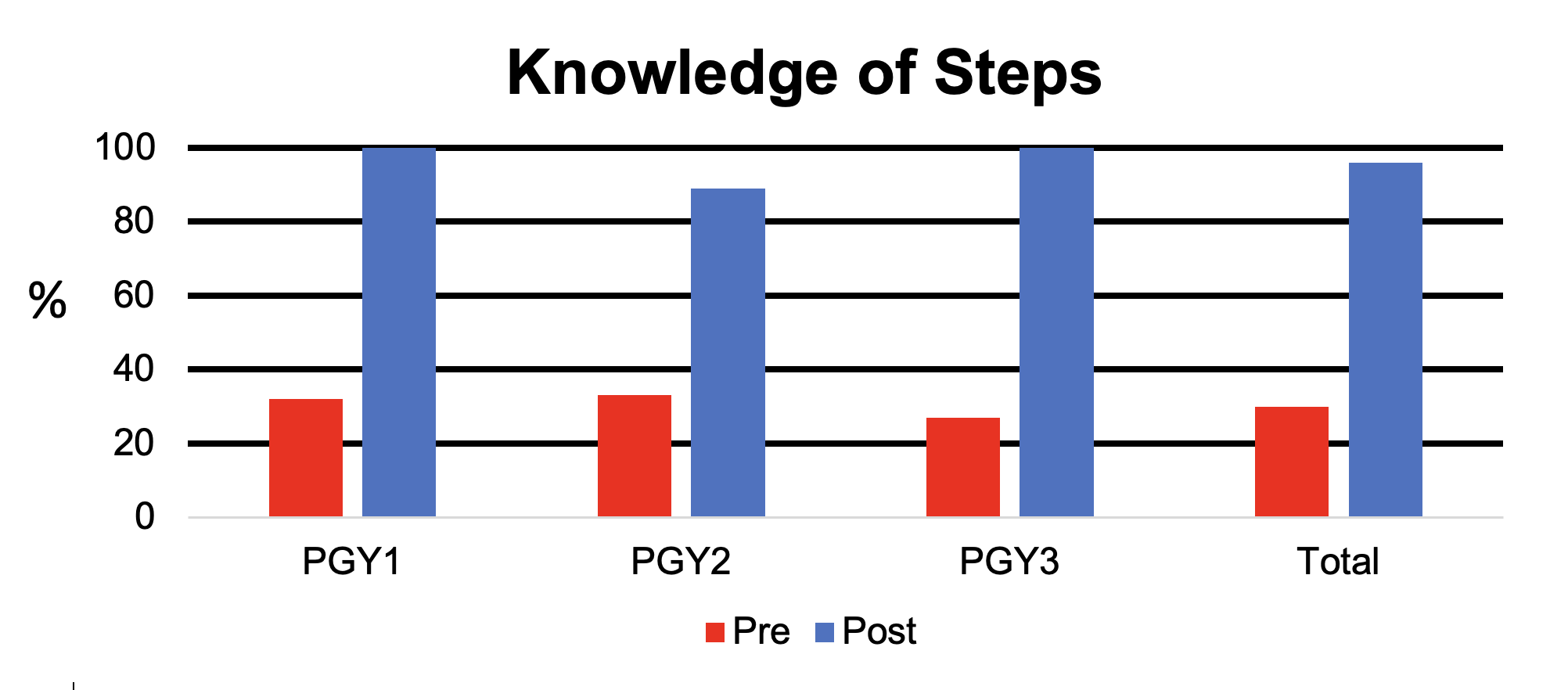
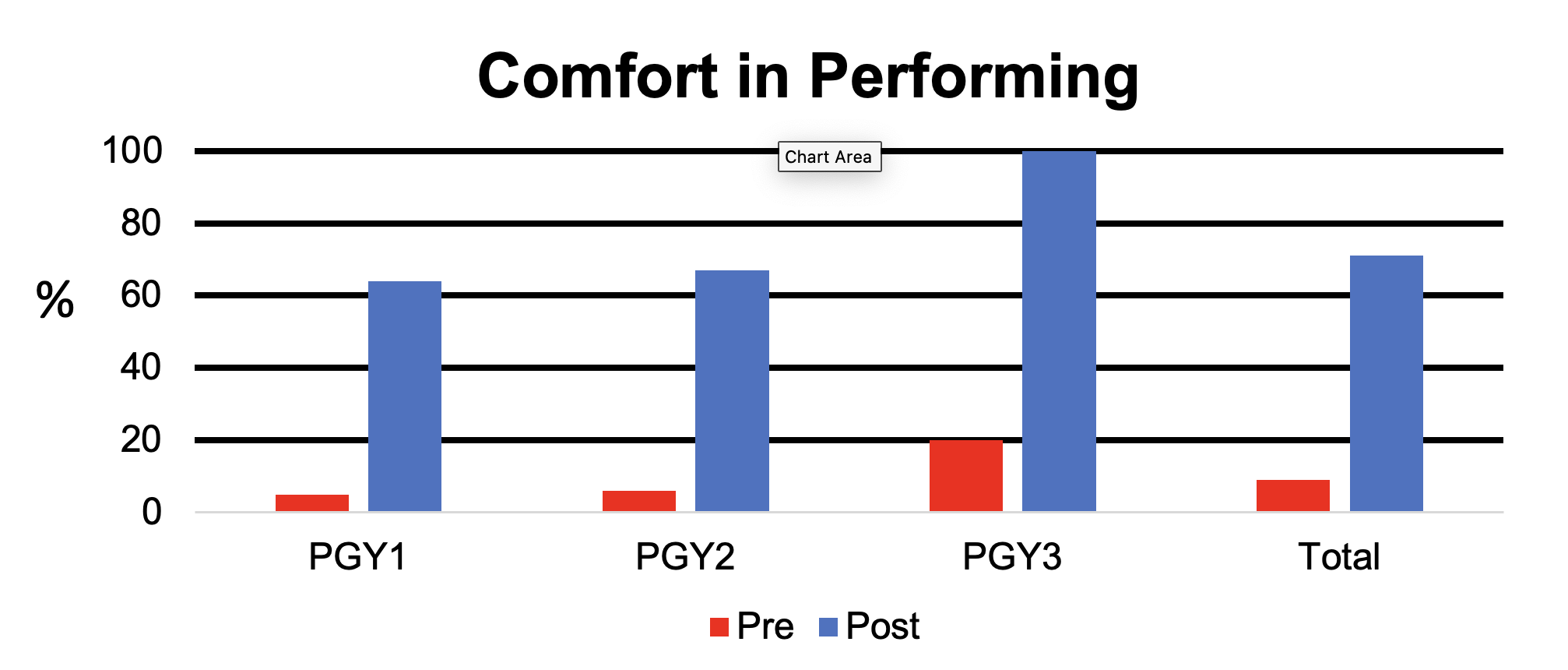
Results: Of the entire program, 57 (70% of a total 82) completed the pre-survey, 24 (42%) completed the simulation, and 7 (29%) completed the checklist simulation. While 88% had witnessed a circumcision in the past, 30% knew the steps, and 9% felt comfortable performing one. After simulation, 96% knew the steps, and 71% felt comfortable. All respondents indicated an increased likelihood to perform a circumcision in the future after simulation. The median checklist score was 75% during the unguided simulation with a range of 60% to 85%.
Conclusion(s): Simulation of the circumcision technique is an effective method to increase exposure and resident’s perceived knowledge and comfortability with the procedure. Short term retention of skills demonstrated during the unguided simulation were lower than expected. Additional work is necessary to increase short term retention of skills and to study the long-term effects of simulation on resident knowledge and patient outcomes.