Children with Chronic Conditions
Children with Chronic Conditions 3
86 - Piloting a Formalized Complex Care Nurse Coordinator Curriculum
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 86
Publication Number: 86.305
Publication Number: 86.305
Mary R. Ciccarelli, Indiana University School of Medicine, Indianapolis, IN, United States; Alyssa Swick, Indiana University School of Medicine, Brownsburg, IN, United States; Natasha Guffey, IU School of Medicine, Indianapolis, IN, United States; Lorena Flaa, Indiana University School of Medicine, Indianapolis, IN, United States

Mary R. Ciccarelli, MD (she/her/hers)
Professor of Clinical Medicine-Pediatrics
Indiana University School of Medicine
Indiana University
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Nurse care coordinators (CCs) are charged with organizing patient needs and facilitating navigation and communication between patients and the health system to improve care delivery. Hiring practices may target the identification of basic CC skill requirements in communication, family-centered care, teamwork, organization, and time management. Once hired, existing curricula focus on principles and goals, more than point-of-care skills. Furthermore, health systems have limited structures to standardize the training of CC nurses to promote the skills needed to efficiently support the complex needs of their patients, as well as navigate complex health systems and community services.
Objective: To develop a standardized coaching model with a formal curriculum for CCs that improves their knowledge and point-of-care skills in the delivery of comprehensive, family-centered, targeted supports for patients with complex needs and their families.
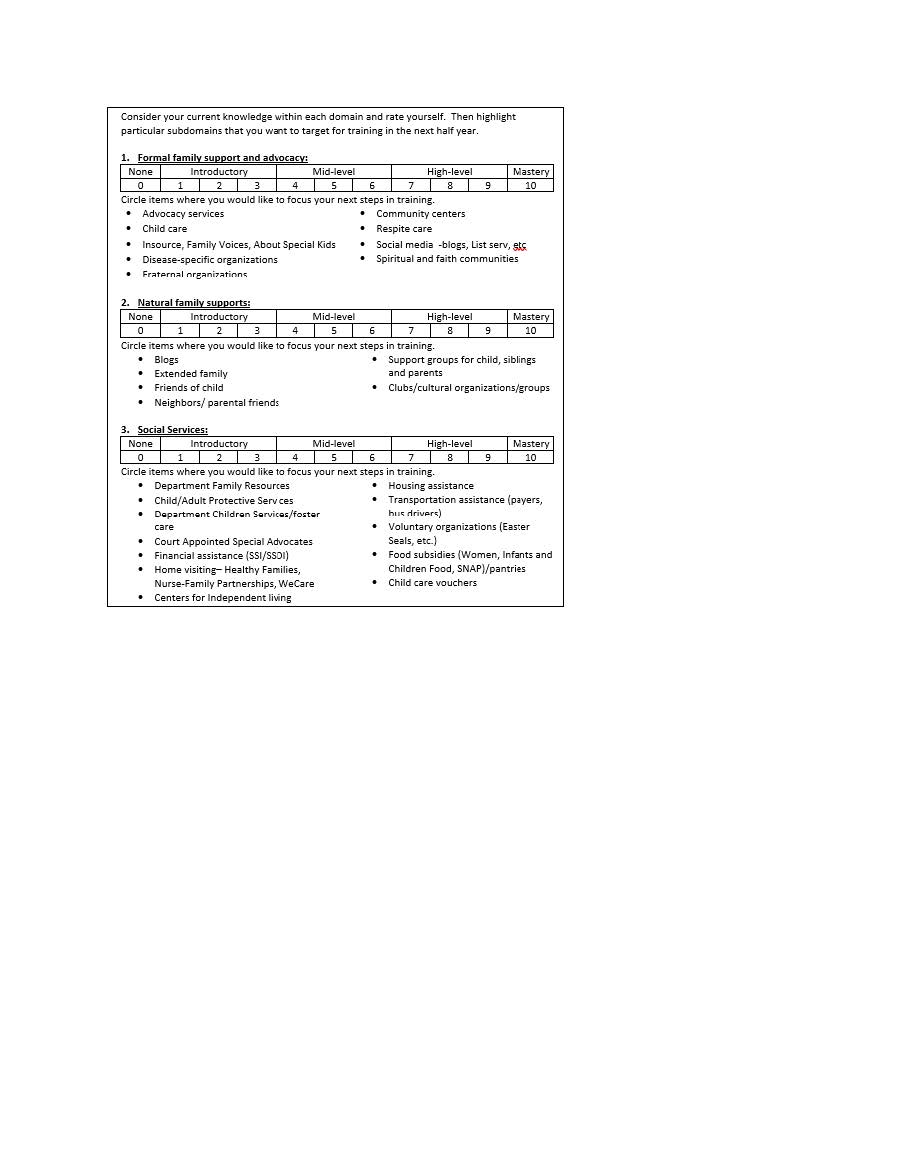
Design/Methods: A coaching model was developed with three training phases: orientation (2 weeks at 6-8 hours per week), high intensity (6 months at 3 hours per week), and a subsequent longitudinal learning collaborative (3 hours per month). (Figure 1) The high intensity training includes a series of weekly didactic sessions (total of 20), plus weekly case-related discussions supported by navigation playbooks. A CC self-assessment survey was developed to measure pre and post levels of knowledge and skill in 16 domains on a scale of 0-10 where 0 = no skill and 10 = mastery. The domains were adapted from a Lucile Packard document of potential services for children with special health care needs, including explanatory examples for each domain. (Figure 2)
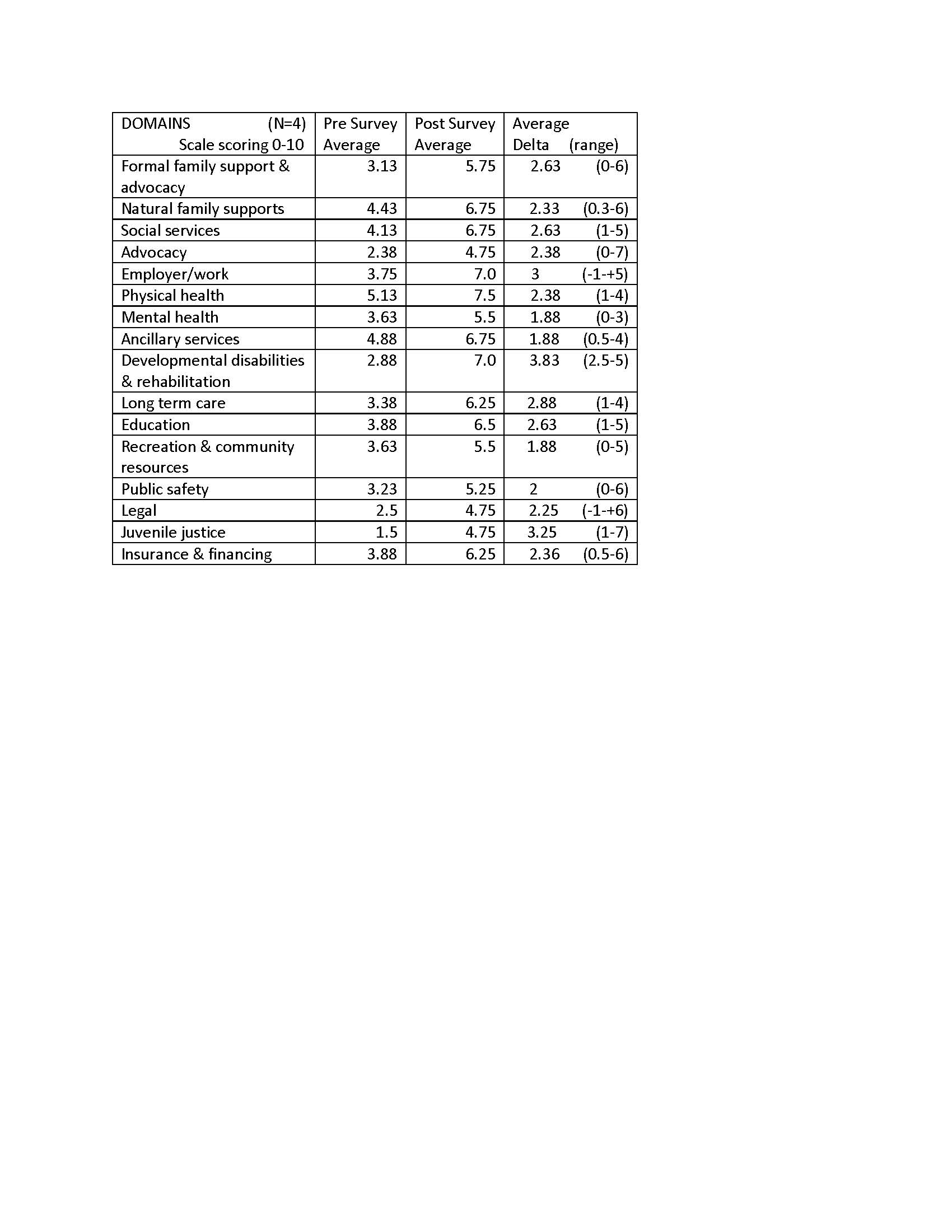
Results: Paired data from 4 CCs indicated a 2.44 point (range 1.07-5.19) increase in individual average scores over an average timespan of 6.75 months (range 3-12 mos). Initial average score was 3.37 or introductory, increasing to 6.06 or mid-level. (Table 1) The three domains with the greatest growth were developmental disabilities and rehabilitation, juvenile justice, and work/employment; the highest absolute scores in post surveys were physical health, work/employment and developmental disabilities, and rehabilitation.
Conclusion(s): Care coordinators within a new formalized coaching program can demonstrate growth in self-confidence regarding their knowledge needed to serve children with special health care needs within a relatively brief time period.