Medical Education: Resident
Medical Education 9: Simulation & Technology 2
519 - Asynchronous Learning Modalities to Enhance High-Acuity Clinical Education: A Randomized Study
Publication Number: 519.327

Chloë E. Nunneley, MD (she/her/hers)
Fellow in Pediatric Hospital Medicine
Boston Children's Hospital/Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Traditional pediatric resident education includes hands-on clinical experiences and in-person didactic lectures. Amid duty hour restrictions, the COVID-19 pandemic, and growing patient complexity, residents have fewer opportunities for real-time educational experiences yet are first responders to high-acuity events. Asynchronous learning can supplement trainees’ clinical knowledge and confidence, but the optimal modality for delivering online content is unknown. Based on experiential learning theory, we hypothesized that knowledge gains and self-confidence would be higher with more interactive modalities (video/simulation), as compared to a static PDF document.
Objective:
We aimed to compare the efficacy of three different asynchronous online educational modalities – 1) PDF document, 2) video, and 3) interactive online case-based simulation – in increasing pediatric residents’ knowledge and confidence in responding to acute inpatient scenarios.
Design/Methods:
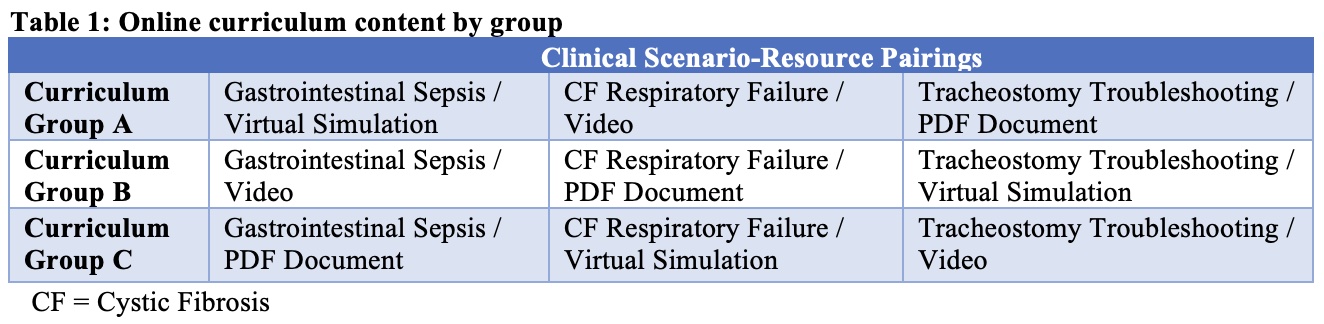
This prospective, randomized study assigned participants from a large pediatric residency program to one of three curricular groups (Table 1). Curricular materials targeting acute clinical scenarios (sepsis, acute respiratory failure, and tracheostomy problems) were developed by study authors, reviewed by faculty content experts, and published on OPENPediatrics (www.openpediatrics.org). Multiple-choice question (MCQ) tests and survey questions assessed knowledge and confidence, respectively, before, immediately after, and two-three months after intervention. Data were analyzed using paired t-tests for MCQ tests and Fisher's exact tests for surveys.
Results:
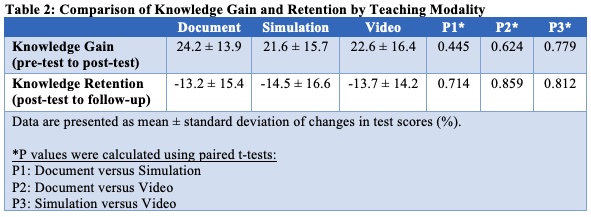
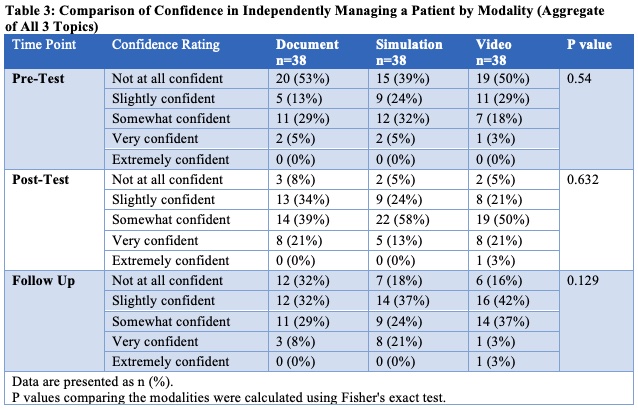
Thirty-eight residents of 145 potential residents were enrolled and 100% completed all components of the study. All three modalities increased residents’ objective knowledge gain, knowledge retention, and subjective confidence across all clinical scenarios. Knowledge and confidence decreased over time, but mean follow-up scores were higher than mean pre-test scores for all modalities (Tables 2 and 3). There were no significant differences in knowledge or confidence gain or knowledge retention by modality or clinical scenario.
Conclusion(s):
Asynchronous educational materials can increase pediatric residents’ confidence and knowledge of the appropriate management of acute events, and these gains can persist over time. All modalities produced similar outcomes, thus, medical educators should feel empowered to develop asynchronous materials of varying format and complexity. Low-cost text or video options may be as effective as resource-intensive modalities such as case-based simulations.