Neonatal Follow-up
NICU Follow Up and Neurodevelopment 6: The NICU Stay and Outcomes
53 - Differential Effects of Asthma on Attention Symptom Trajectories in Term and Preterm Children
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 53
Publication Number: 53.446
Publication Number: 53.446
Jonathan S. Litt, Beth Israel Deaconess Medical Center, Boston, MA, United States; Henning Tiemeier, Harvard T.H. Chan School of Public Health, Boston, MA, United States

Jonathan S. Litt, MD, MPH, ScD (he/him/his)
Neonatologist
Beth Israel Deaconess Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background: Cross-sectional analyses reveal an association between pediatric asthma diagnosis and attention deficit/hyperactivity disorder (ADHD). Preterm infants are at increased risk for both asthma and ADHD compared to term-born peers. The effect of asthma on ADHD symptoms over time is unclear, and the differential effect among higher-risk preterm infants is unknown.
Objective: We aimed to describe the longitudinal effect of asthma on ADHD symptoms in childhood and test if there is a differential effect among higher-risk preterm infants compared to term-born peers.
Design/Methods: We used longitudinal data from the Generation R birth cohort for our secondary data analysis. Participants were born in Rotterdam, Netherlands between April 2002 and January 2006. The primary outcome was Attention Problem subscale t-scores of the Child Behavior Checklist measured at 3, 5, 9, 14, and 18 years of age. The primary predictor was ever having an asthma diagnosis. Birth before 37 weeks (preterm, PT) was included as an effect modifier. Covariates included child sex, maternal age, parity, psychological health, smoking status, marital status, and ethnicity, and household income, family functioning, and parenting competence. We used generalized linear models to estimate the fixed effect of time on Attention Problem scores and the between-subject effects of asthma diagnosis and PT birth.
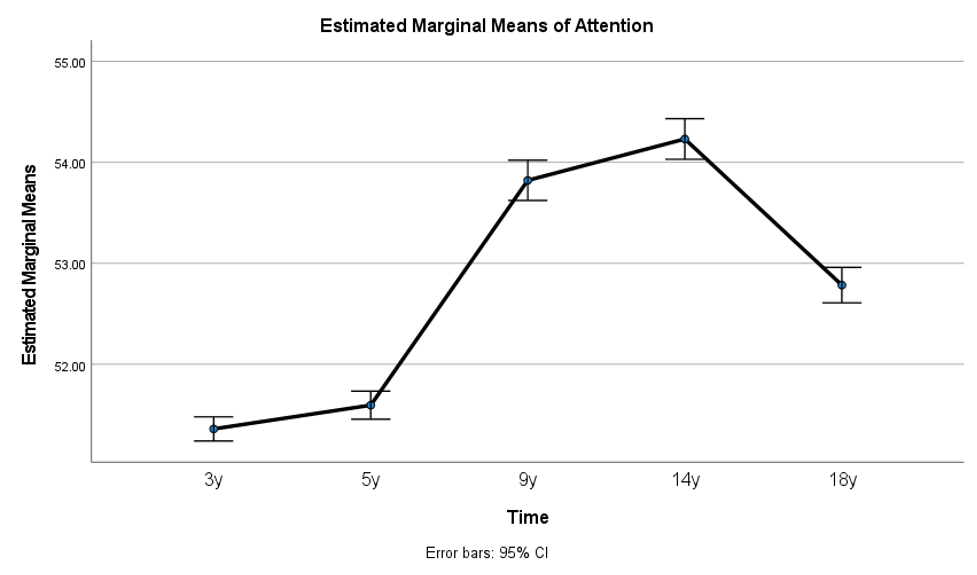
Results: There were 3401 children with complete outcomes data at all time points. Mean Attention Problem scores ranged from 51.5 (SD 3.3) at age 3 to 54.4 (SD 5.4) at age 14. Three-hundred and forty (10%) children had an asthma diagnosis and 183 (5.4%) were born PT. Average Attention Problem scores changed significantly over time (Figure 1). The pattern of Attention Problem scores differed modestly between children with and without asthma (Figure 2), with higher scores for those with asthma compared to those without at age 14. The effect of asthma on Attention Problem scores was significantly greater for PT children compared to term-born peers, driven by notably higher scores at age 14 for PT children with asthma compared to those without.
Conclusion(s): Attention Problem scores change during childhood, increasing in school-age and peaking in early adolescence. Peak scores are higher for children with an asthma diagnosis; this effect is greater for children born PT. Further work is needed to ascertain the functional impact of these differential symptom trajectories and identify opportunities for intervention to reduce associated morbidity.
.png)
