Neonatal Pulmonology
Neonatal Pulmonology 5: NICU Practices
152 - Massive Pulmonary Hemorrhage according to the Therapeutic Strategies for Patent Ductus Arteriosus in Extremely Low Birth Weight Infant
Publication Number: 152.437
Ju Sun Heo, MD, PhD
Assistant Professor
Korea University College of Medicine
Seoul, Seoul-t'ukpyolsi, Republic of Korea
Presenting Author(s)
Background:
Massive Pulmonary hemorrhage (MPH) is a fatal event associated with significant morbidity and mortality. Increased pulmonary blood flow due to left-to-right shunting through patent ductus arteriosus (PDA) can give rise to pulmonary edema, microvascular injury and eventual capillary hemorrhage. When MPH is precipitated by a hemodynamically significant PDA, it is important to consider treating the PDA pharmacologically.
Objective:
We compared MPH and MPH-related outcomes of infants treated conservatively without any intervention and those of infants managed by other therapeutic strategies in extremely low birth weight (ELBW) infants with PDA.
Design/Methods:
A prospective cohort study for 4,910 ELBW infants from the Korean Neonatal Network (KNN) database from 2013 to 2020 was conducted. The KNN is a nationwide very low birth weight infant registry that has been collecting clinical data from 76 neonatal intensive care units across South Korea. These infants were classified into five groups according to the presence of PDA-related symptoms and therapeutic treatment strategy: no PDA group, prophylactic treatment (PT) group, pre-symptomatic treatment (PST) group, symptomatic treatment (ST) group, and conservative treatment (CT) without any intervention group.
Results:
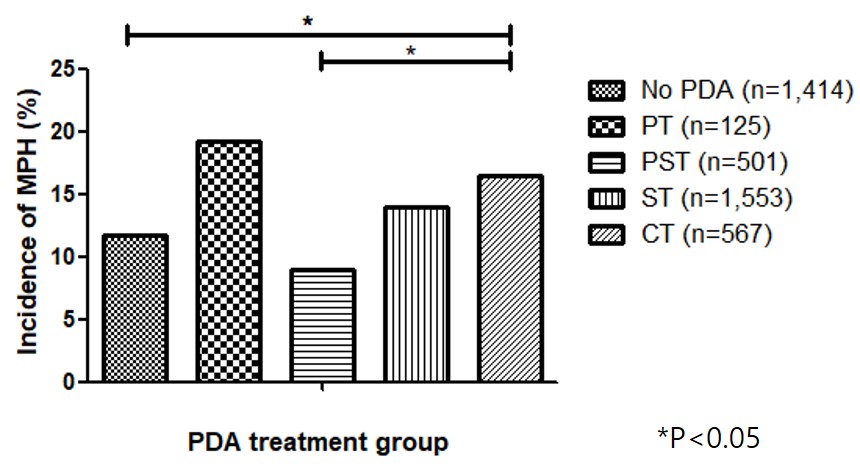
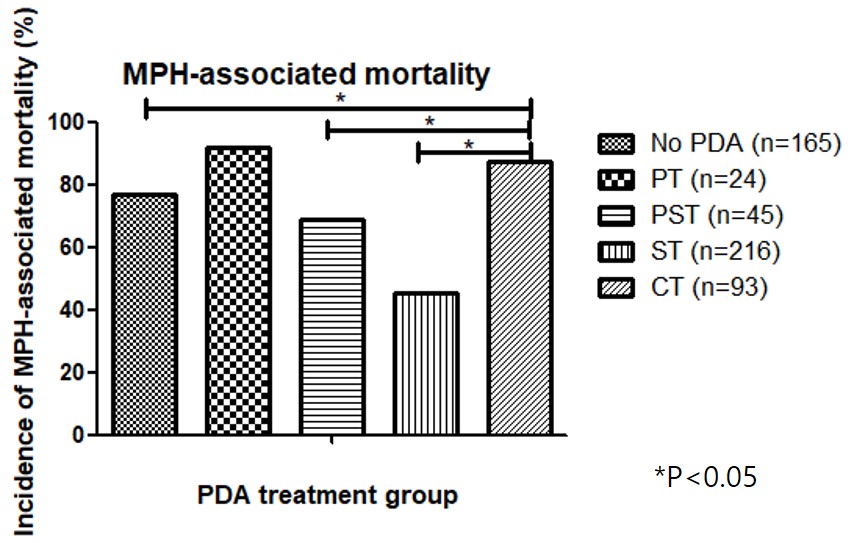
1. The incidence of MPH was 11.1% (543 of 4,910) and MPH-associated mortality rate was 66.1% (359 of 543).
2. The incidence of MPH in the CT group was significantly higher than that in the PST group (16.4% vs. 9.0%). And MPH-associated mortality in the CT group was higher than that in the PST or ST group (87.1% vs. 68.9% or 45.4%). In multivariable logistic regression analysis, the risk of MPH was decreased only in the PST group (adjusted odds ratio [aOR] = 0.461, 95% confidence interval [CI] = 0.294-0.723) compared with the CT group. The risk of MPH-associated mortality was decreased in the PST group (aOR = 0.216, 95% CI = 0.071-0.652) and ST group (aOR = 0.087, 95% CI = 0.038-0.197) compared with the CT group.
3. Among the survival infants from MPH, the risk of composite outcome of death or severe bronchopulmonary dysplasia was decreased in the ST group (aOR = 0.255, 95% CI = 0.085-0.763) compared with the CT group.
Conclusion(s):
In ELBW infants, who are at highest risk of MPH and related morbidities and mortality, even less interventional approach for PDA can be allowed; the early targeted pharmacological management might be necessary if they met the criteria for the risk of becoming clinically significant PDA, based on echocardiographic parameters.