Neonatal Follow-up
NICU Follow Up and Neurodevelopment 6: The NICU Stay and Outcomes
52 - Association of Unplanned Extubations on Neurodevelopmental Outcomes in Very Low Birthweight Infants
Publication Number: 52.446

Alexandra J. Golden, B.S. (she/her/hers)
Medical Student
Vanderbilt University School of Medicine
Boca Raton, Florida, United States
Presenting Author(s)
Background:
Unplanned extubations (UEs) are associated with a nearly one-week longer duration of mechanical ventilation (MV) and the length of MV is associated with poorer neurodevelopmental outcomes (NDO). Despite these associations, the relationship between UEs and NDO has not been studied.
Objective:
To determine if UEs in the Neonatal Intensive Care Unit (NICU) are associated with poorer NDO, specifically within the motor domain.
Design/Methods:
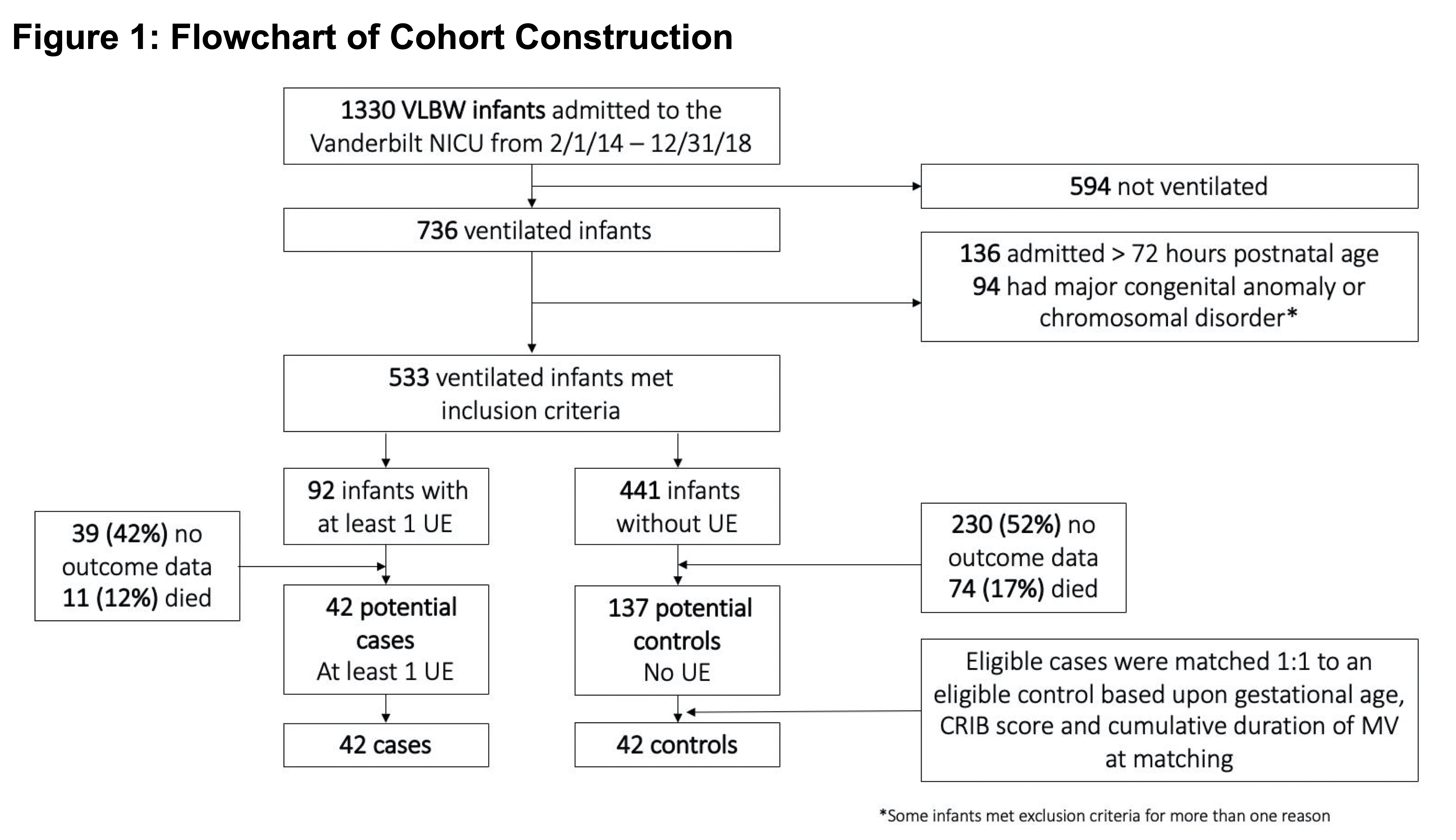
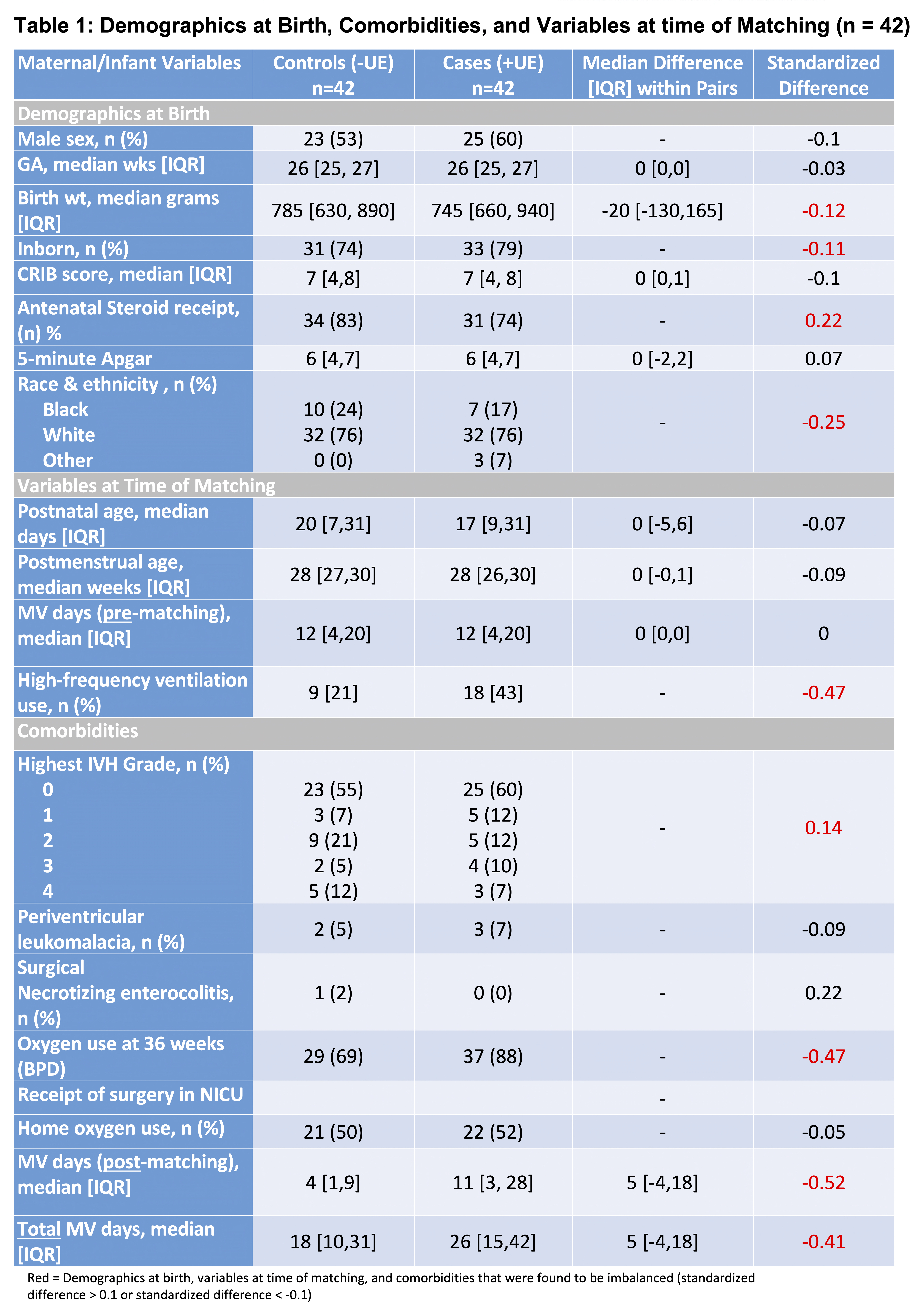
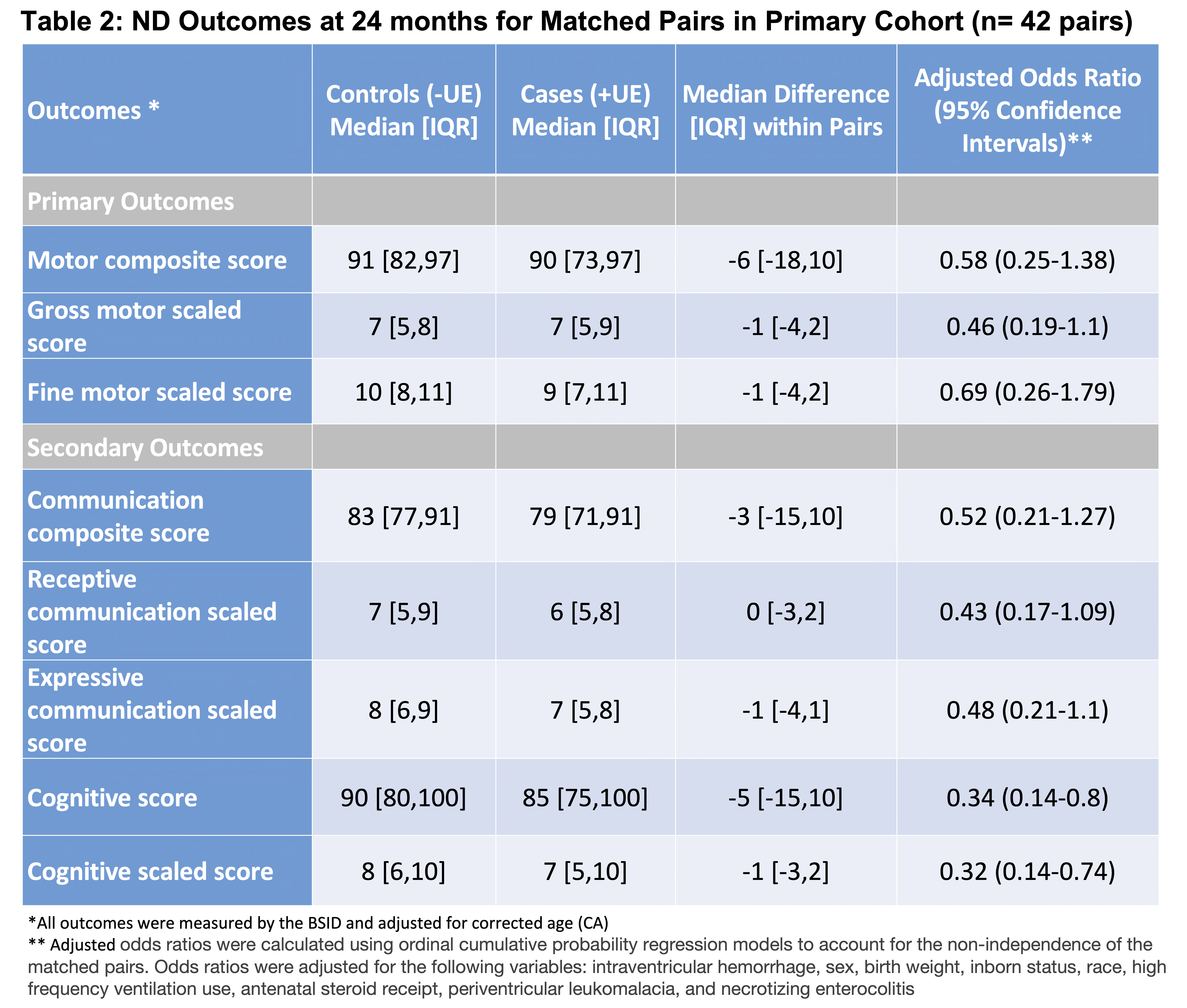
We conducted a retrospective observational matched cohort study in the 98-bed, level IV regional academic NICU of the Vanderbilt University Medical Center (VUMC) from 2014-2018. All very low birth weight (VLBW) infants (< 1500 g at birth), admitted within 72 hours of birth, without chromosomal or congenital anomalies, who received MV through an endotracheal tube (ETT) for ≥1 hour, and had neurodevelopmental follow-up data at VUMC were included. The primary exposure was the occurrence of one or more UEs defined as any removal of an ETT that the medical team did not plan in advance for removal. We measured motor outcomes between 20-30 months of age using the Bayley Scales of Infant Development (BSID-III). Cases (+UE) were matched 1:1 using a greedy nearest-neighbor matching algorithm based upon gestational age, Clinical Risk Index for Babies score, and cumulative duration of MV at matching. Descriptive statistics and multivariable ordinal cumulative probability regression models were used to compare groups and evaluate outcomes.
Results:
During the study period, 179 infants met study inclusion criteria and had NDO testing available. Of these 179 infants, 42 (23%) had one or more UEs and a total of 42 matched pairs were formed (Figure 1). Cases and controls showed improved balance after matching. Infants with a UE had a longer post-matching duration of MV (median 11 vs. 4 days) compared to matched controls (Table 1). Cases had lower BSID-III motor composite scores with median difference [IQR] within matched pairs of -6 [-18,10]. After adjusting for confounding, this difference was not significant (aOR = 0.58, 95% CI = [0.25 1.38]). Gross and fine motor scores and secondary NDO are shown in Table 2.
Conclusion(s):
We did not find a significant association between UEs in VLBW infants and BSID-III motor outcomes at 24-months postnatal age. However, consistent with prior studies, we found that infants who had one or more UEs in the NICU had longer MV duration than those who did not. Given the known detrimental effects of increased MV duration on NDO and our study’s relatively small sample size, larger studies are needed to ensure that UEs are not associated with adverse NDOs.