Neonatal General
Neonatal General 10: Outcomes
65 - Maternal mental health conditions affect newborn resilience and neuromotor function
Publication Number: 65.429
- MK
Merrick Kasper, B.A. Biology
Clinical Research Coordinator
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background:
It is increasingly recognized that maternal mental health (MH) can influence prenatal brain development and subsequent neurobehavior in offspring. Maternal populations diagnosed with MH disorders can be at increased risk for stress during the pregnancy period, potentially impacting fetal health into the neonatal period. Despite this significant risk, the screening and diagnosis of MH disorders in pregnancy remain limited, with even fewer treatment options available. Furthermore, neurodevelopmental outcomes of infants born to pregnant women experiencing MH problems remains largely unstudied.
Objective:
To investigate the association between maternal mental health conditions in pregnancy and neurodevelopmental outcomes of newborns.
Design/Methods:
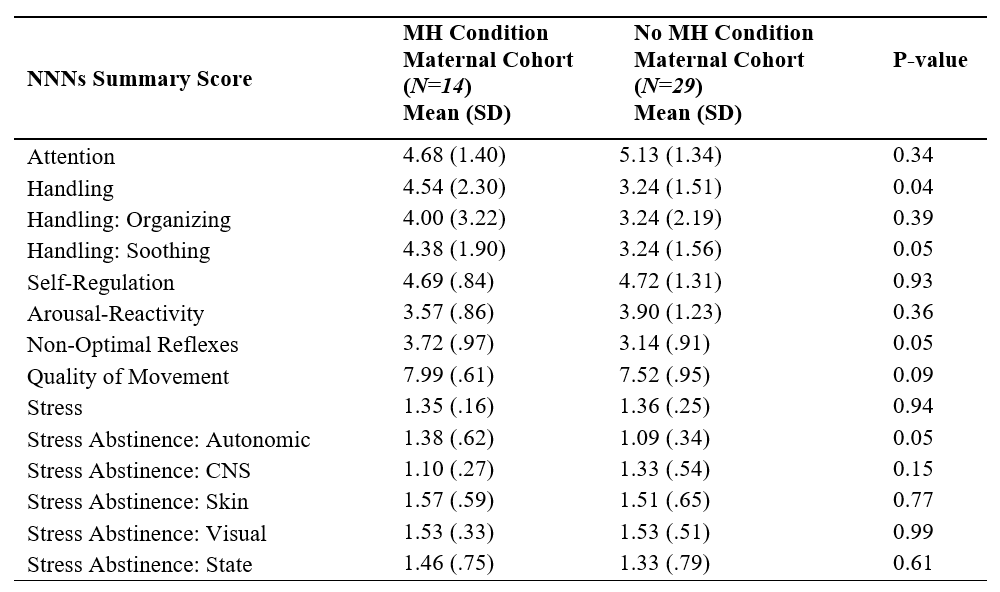
We recruited pregnant women with and without MH conditions into a prospective observational study to elucidate maternal health and infant outcome. Prenatal maternal mental health diagnosis was abstracted from the medical record. Maternal mental distress was assessed in pregnancy using validated questionnaires: the Edinburgh Postnatal Depression Scale (EPDS), Perceived Stress Scale (PSS) and Spielberger Trait Anxiety Inventory (STAI); scores were considered elevated if above the following predefined threshold. Infant outcomes were assessed using the NeoNatal Neurobehavioral Scale (NNNs-II) within the first month of life.
Results:
We enrolled 43 mother-infant dyads; of which 14 (32%) pregnant women were diagnosed with a MH condition (depression/major mood disorder: 9; anxiety: 9 and PTSD: 2); of whom 10 (71%) were receiving treatment. Pregnant women with a MH condition had significantly higher stress and anxiety scores compared to those without a MH condition (Figure 1); 50% of pregnant women with MH conditions scored above threshold for both anxiety and stress, compared to only 3-10% of those without MH conditions (Table 1). Infants of mothers with known MH conditions required significantly more special handling, with notable trends toward greater non-optimal reflexes and higher stress abstinence scores (Table 2).
Conclusion(s):
We describe a significant number of pregnant women experiencing elevated levels of stress and, especially in women with diagnosed MH conditions. Furthermore, offspring of pregnant women with MH conditions demonstrate altered neonatal neurobehavioral regulation, in the setting of ongoing elevated mental distress. This highlights the need for continued preventive mental health screening and treatment in the perinatal period as well as the importance of ongoing neurodevelopmental surveillance of affected offspring. 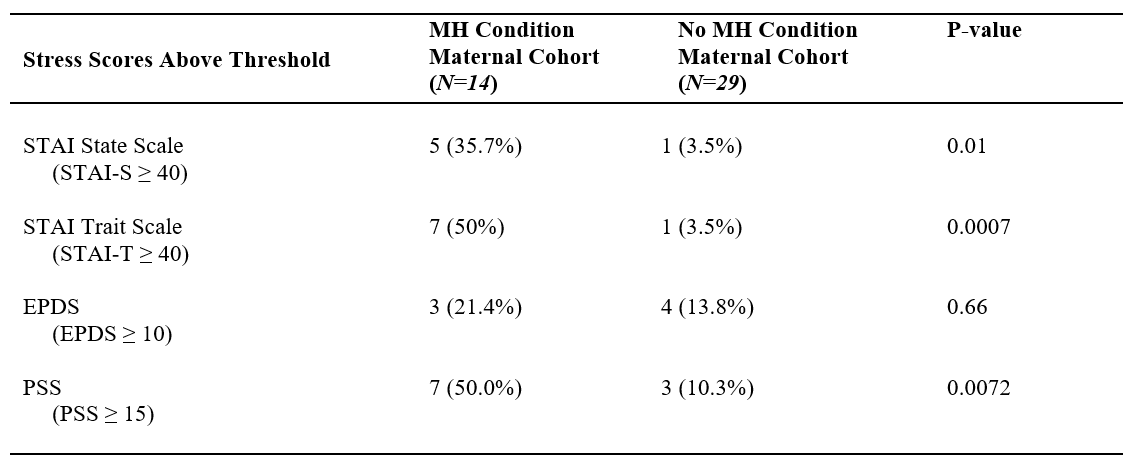
.png)
