Neonatal Quality Improvement
Neonatal Quality Improvement 6
207 - Improving Procedural Pain Management in a Level III Neonatal Intensive Care Unit
Publication Number: 207.44

Pavani Chitamanni, MBBS (she/her/hers)
Resident Physician
State University of New York Downstate Medical Center College of Medicine
Brooklyn, New York, United States
Presenting Author(s)
Background: Neonatal pain can have negative short and long-term consequences, including poor cognitive and neurobehavioral outcomes. Improving knowledge of neonatal pain management among the NICU staff and adopting its implementation into daily practice is vital.
Objective: To increase the use of neonatal pain management interventions by NICU staff to more than 70% within a three-month period.
Design/Methods:
We used the plan-do-study-act (PDSA) problem-solving approach. Our interventions were NICU staff education using presentations and flyers, weekly interdisciplinary meetings to reinforce the guidelines for neonatal pain management, increased accessibility of commonly used pharmacological agents and their dosages (Figure 1). Data was collected through individual surveys. Our outcome measure was the percentage of NICU healthcare staff who implement neonatal pain management interventions >70% of the times. Our process measure was the number of educational interventions and meetings with the staff. Our balancing measure was delay in patient care. Chi-squared test for proportions was used for analysis of pre- and post-intervention outcomes.
Results:
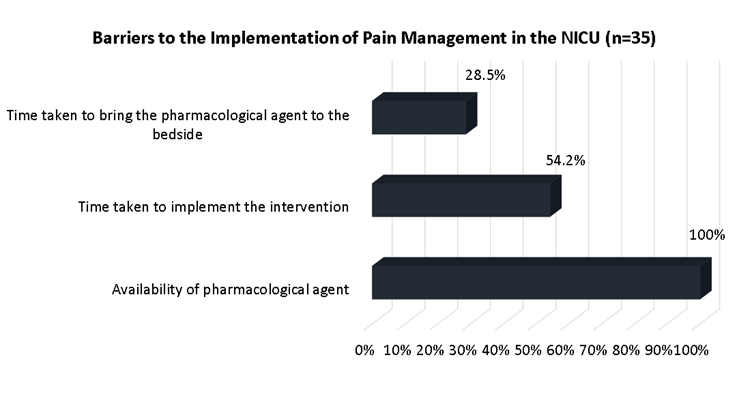
Pre-intervention data was collected from 51 NICU staff (35 nurses and 16 house staff) and postintervention data from 35 NICU staff (26 nurses and 9 house staff). Over >45% of the NICU staff perform three or more procedures per day. The percentage of NICU staff employing non-pharmacological measures and topical analgesics during more than 70% of skin-breaking procedures increased from 64% (33/51) and 5.8% (3/51) respectively to 82% (29/35) and 48.5% (17/35). Table 1 describes improvement in multiple areas along with their p-value. The percentage of NICU staff who believed that they were adequately trained in neonatal pain management increased from 17.6% (9/51) before to 62.8% (22/35). Common barriers to implementing pain management reported were the availability of pharmacological agents (35/35, 100%) and the time taken to implement the intervention (19/35, 54.2%) (Figure 2). Majority (19/35, 54.2%) of the staff reported requiring < 1 minute to implement non-pharmacological pain management interventions. Only a small percentage (4/35, 11%) reported that implementing pain management interventions has delayed patient care.
Conclusion(s):
We were able to increase the use of procedural pain management modalities in the NICU, using QI methodologies and with interdisciplinary cooperation. To further increase the implementation of pain management interventions, additional PDSA cycles along with increasing the availability of pharmacological agents are warranted.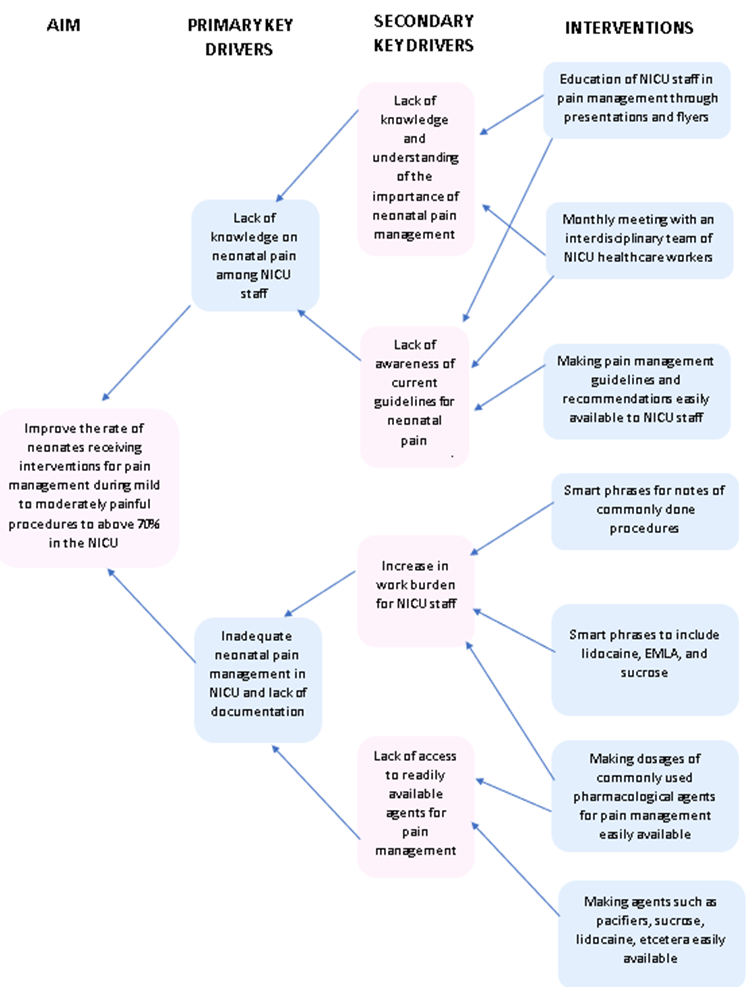
.png)
