Neonatal General
Neonatal General 11
80 - Utility of Ultrasound Guided Lumbar Puncture in Newborn Infants by Physicians at Different Levels of Training
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 80
Publication Number: 80.43
Publication Number: 80.43
Jane Huang, University of Southern California/Keck School of Medicine of USC, MONTCLAIR, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Amy Yeh, University of Southern California, Keck School of Medicine, Los Angeles, CA, United States
.jpg)
Jane Huang, DO (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Southern California/Keck School of Medicine of USC
MONTCLAIR, California, United States
Presenting Author(s)
Background: Lumbar puncture (LP) is one of the most common procedures performed in the neonatal intensive care unit. Despite being an essential diagnostic procedure, failure rate resulting from inability to obtain CSF or traumatic LP is reported to be as high as 30-50%. Traditionally, LP has been performed with palpation of landmarks; however, there are emerging data that describe the improvement in success with the use of ultrasound (US) by US trained physicians to either mark the area of interest prior to needle insertion (static) or to guide LP in real time (dynamic). The success rate and rate of traumatic puncture of US guided LP performed in neonates or infants by physicians with various experiences are not known.
Objective: To assess the feasibility of dynamic and static US guided LPs by physicians at different levels of training.
Design/Methods: Neonates and infants admitted to the NICU at LAC+USC Medical Center starting in May 2022 who required LP were enrolled. LPs were performed by Pediatric residents, NICU fellows and attendings. All Pediatric residents and NICU fellows did not have prior experience in US guided LP and training was provided prior to the procedure. No US guided LP has been performed in the unit prior to the start of the study. Dynamic US guided LPs were initially performed but the static technique was introduced to compare success rate. Successful LP was considered when CSF was obtained. Traumatic puncture was defined as red blood cells count greater than 10,000/mm³.
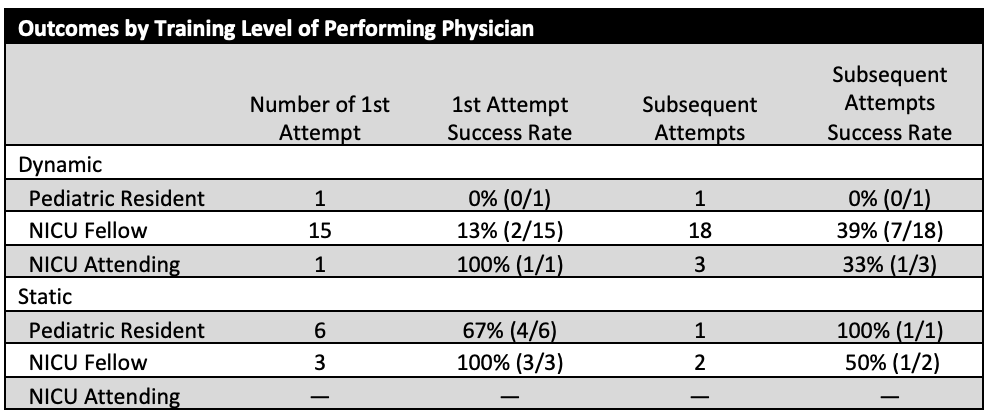
Results: Seventeen dynamic LPs were performed in neonates with median gestational age of 38+1/7 weeks and median birthweight of 3001 grams. First attempt and overall success rate were 24% (4/17) and 65% (11/17), respectively. Traumatic LP rate was 45% (5/11). Nine static LPs were performed in neonates with median gestational age of 38+4/7 weeks and median birthweight of 3235 grams. First attempt and overall success rate were 78% (7/9) and 100% (9/9), respectively. Traumatic LP rate was 44% (4/9). Total number of attempts performed by physicians at different training level and their success rate are shown in the Table 1. Reasons for traumatic puncture include minimal CSF within thecal sac, presence of large epidural hematoma from prior attempt, and excessive patient movement.
Conclusion(s): Our study demonstrates that the use of US to assist in LP is feasible in physicians at various levels of training. Dynamic US guided LP may be more difficult in physicians with no prior experience in US compared to static US guided LP. Continued training in US and development of sedation protocol may improve future successful rate.