Quality Improvement/Patient Safety: All Areas
QI 4: Inpatient QI/Patient Safety
229 - Capturing ‘Gut’ Instinct: Implementation of a Clinician Concern Tool for Preventing Unrecognized Deterioration in Hospitalized Children
Publication Number: 229.45

Meghan M. Galligan, MD, MSHP (she/her/hers)
Assistant Professor of Clinical Pediatrics
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Unrecognized deterioration poses a significant risk of harm to hospitalized children. ‘Gut’ instinct can help detect deterioration, but tools to capture this are not well described.
We designed a ‘clinician concern’ process to enhance detection and response to deterioration outside the intensive care unit (ICU). Across February 2021-2022, we implemented the process on 4 pilot units.
Objective:
This study aimed to assess implementation to guide process design and spread.
Design/Methods:
The clinician concern process asks nurses to subjectively assess deterioration risk in the electronic health record alongside vital signs using a 4-point scale with embedded decision support. (Figure 1)
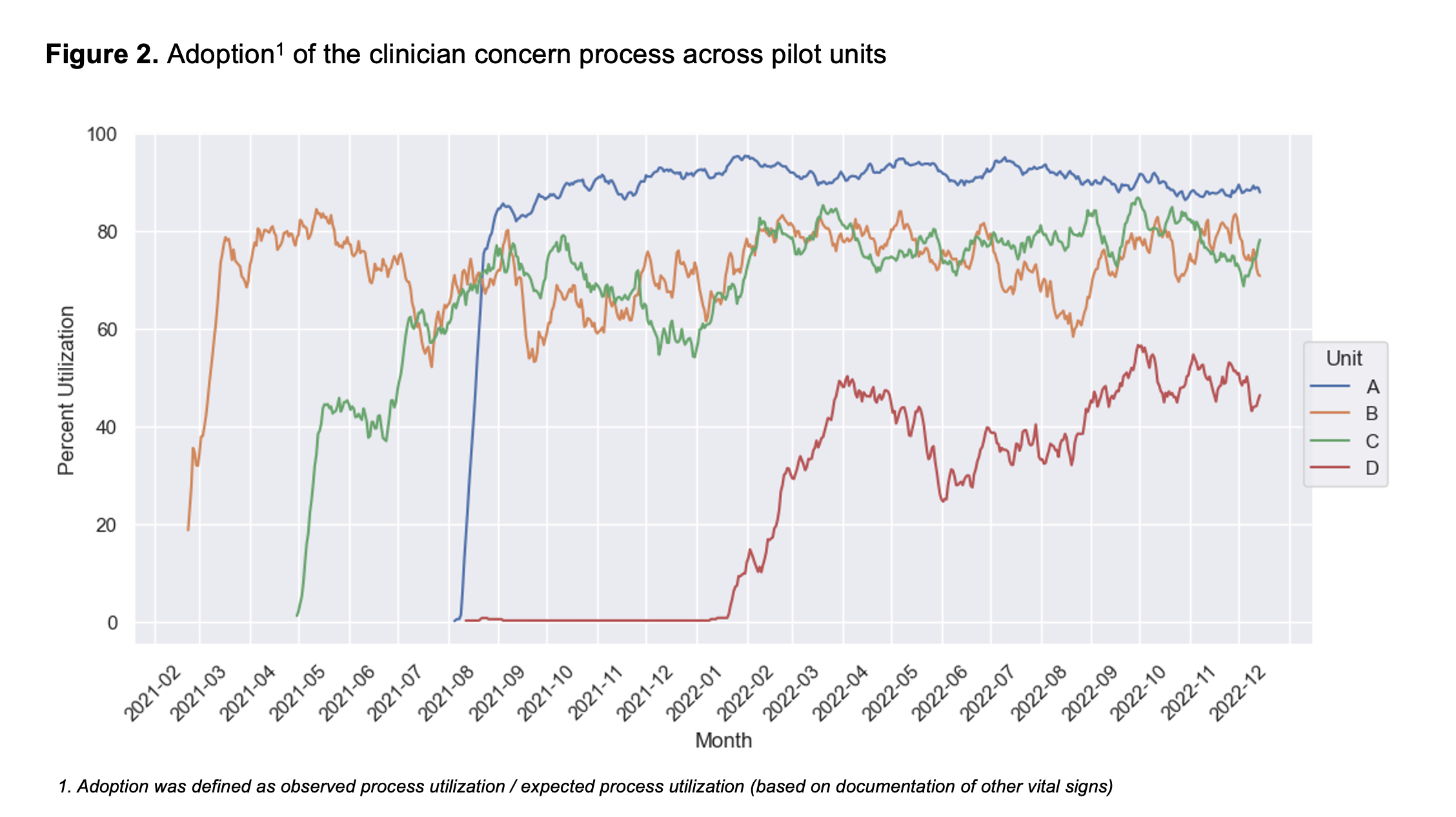
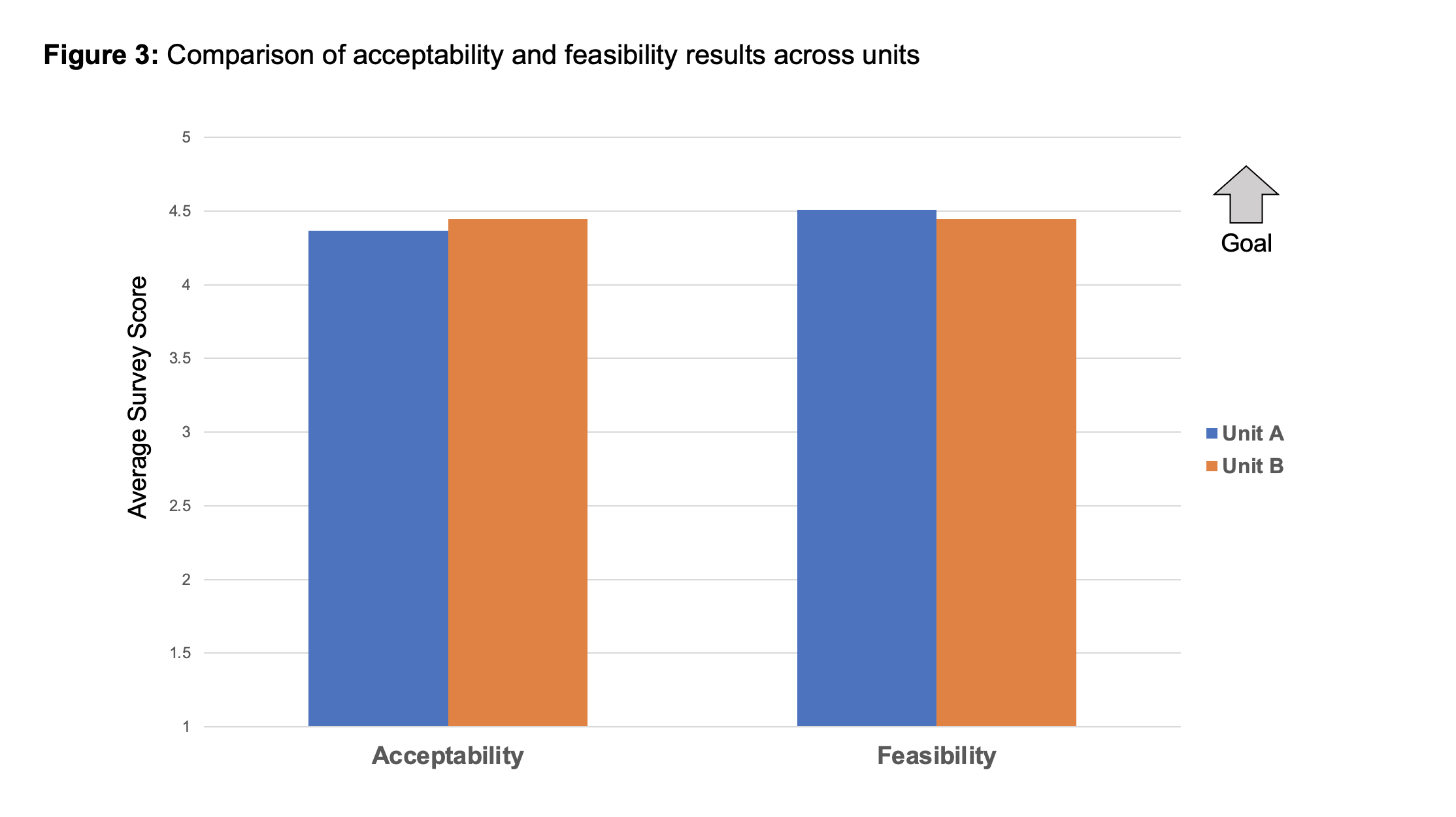
We assessed the following pilot outcomes: adoption; reach; acceptability; and feasibility. To evaluate adoption, we compared observed vs expected process use based on vital sign documentation. We compared daily adoption rates during quarter 3 of each pilot using Kruskal-Wallis testing. We assessed reach, acceptability, and feasibility using a nurse feedback survey. A priori, we selected 2 units (A, B) to survey based on team partnerships. The survey was conducted after ³12 months of the pilot on both units. The survey included the following items, adapted from implementation instruments: ‘I am aware of the clinician concern pilot’ (reach); ‘I like the clinician concern process’ (acceptability); and ‘The clinician concern process seems feasible’ (feasibility). Reach was assessed as a binary yes/no outcome; acceptability and feasibility were assessed via a 5-point Likert scale. Results were compared across units using Fisher’s exact test (reach results) and Mann-Whitney testing (acceptability and feasibility results).
Results:
Adoption varied across units (Figure 2), with significant differences in average daily adoption during quarter 3 (Unit A: 92%; B: 66%; C: 64%; D: 46%; p=0.00). A total of 93 nurses responded to the feedback survey (A: n=73; B: n=20) with an 63% average response rate. Reach was significantly higher on Unit A than B (78% reported awareness vs 45%, p=0.01). Both units reported favorable acceptability (A: 4.37, B: 4.43; p=0.87) and feasibility (A: 4.51, B: 4.44; p=0.74) (Figure 3). In qualitative feedback, nurses from all units described the process as easy to use, empowering, and helpful for triggering huddles.
Conclusion(s):
A clinician concern process pilot had variable adoption but was overall well received by nurses. Variable pilot awareness may have contributed to adoption differences. Future study will evaluate process impact on patient care.
.png)