Neonatal Quality Improvement
Neonatal Quality Improvement 6
206 - Central Line-Associated and Healthcare-Associated Bloodstream Infection Rates Increased Unexpectedly in the University of Utah Neonatal Intensive Care Unit
Publication Number: 206.44
- MN
Mark Nolan, MD
Fellow
University of Utah Division of Neonatology
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
Central line-associated blood stream infections (CLABSI) are associated with both increased morbidity and mortality in the neonatal intensive care unit (NICU). Significant efforts have been made to reduce CLABSI rates nationwide, ranging from bedside caregiving procedures to human factors and systems engineering strategies. After an extended period of nearly three years with zero CLABSI events in the University of Utah NICU, the CLABSI and bloodstream infection (BSI) rates appeared to increase. This unexpected change warranted further investigation to determine if infection prevention efforts or further process changes are indicated.
Objective:
The objective of this study is to determine if the detected increase in CLABSI and BSI rates is a statistically significant change by analyzing CLABSI and BSI rates over the past decade.
Design/Methods:
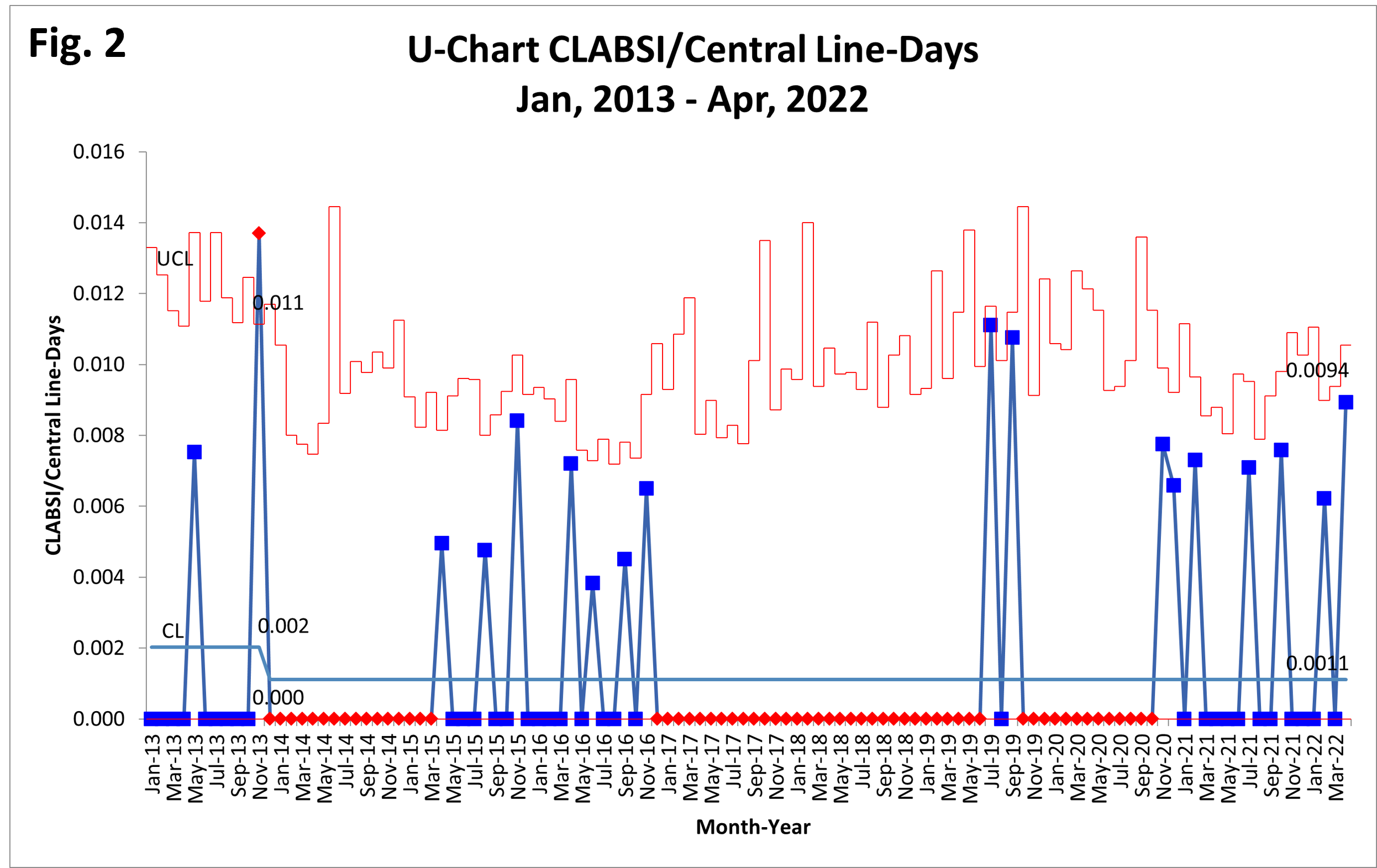
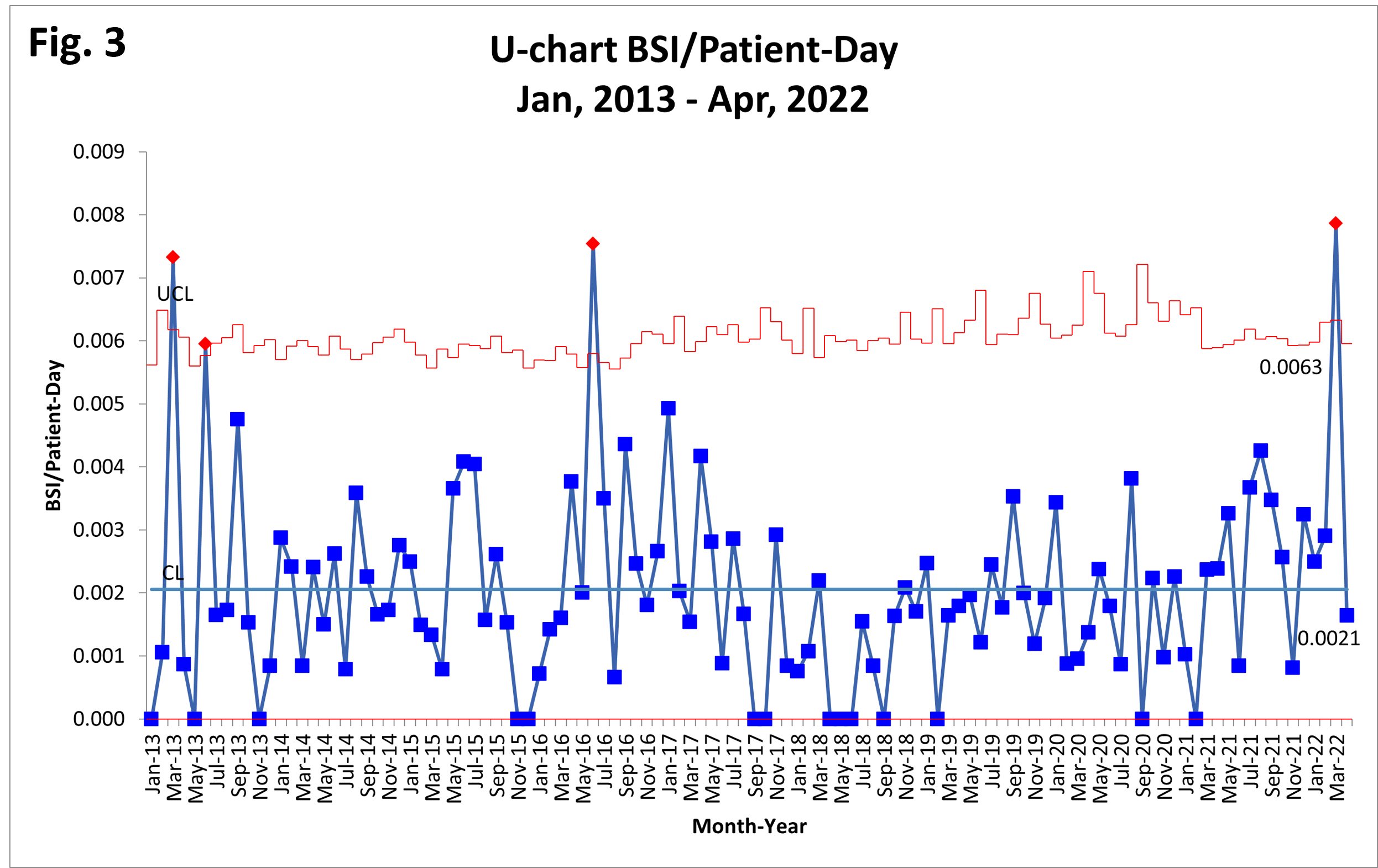
CLABSI and BSI data were extracted from reportable Centers for Disease Control National Healthcare Safety Network data for the period January, 2013, through April, 2022. Data were analyzed using QIMacros 2018 (KnowWare Int’l, Inc., Denver, CO) and healthcare special cause rules for statistical process control chart significance. Days between CLABSI events were plotted on a g-chart (Fig 1). CLABSIs per line-day (Fig 2) and BSIs per patient-day (Fig 3) were plotted on u-charts.
Results:
Average days between CLABSI events increased from 126 in 2013 to nearly 500 in 2016, then fell to fewer than 90 days and have remained constant since November, 2020 (Fig 1). The u-chart (Fig 2) demonstrates three detected runs of zero CLABSI/line-day/month; one special cause signal reached statistical significance, indicating an increase in the CLABSI rate. In contrast, BSI/patient-day (Fig 3) demonstrates no statistically significant improvement signals and four discrete months with special cause increases in BSI events; there were no sustained changes in BSI rate over time.
Conclusion(s):
Concern for an increase in CLABSI rate was confirmed and found to be statistically significant in an analysis of days between CLABSI events and in an analysis of month-to-month CLABSI rates. There was no statistically significant change sustained in BSI rate over the same time period. Additionally, BSI rate demonstrated wide month-to-month variability. Further study of CLABSI prevention practices is warranted to help decrease the incidence of healthcare associated infections in the NICU. BSI rate may represent an additional measure to study..png)