Neonatal Pulmonology
Neonatal Pulmonology 5: NICU Practices
149 - Utilization of Non-Invasive Ventilation in the Management of Pneumothorax in near-term and term neonates is Less Resource Intensive in the United States
Publication Number: 149.437
- KD
Keyur Donda, MD
Assistant professor and Associate fellowship program director
University of South Florida
Brandon, Florida, United States
Presenting Author(s)
Background:
Pneumothorax (PTX) remains a significant cause of morbidity in newborns. Previous studies on neonatal PTX had small sample sizes or were from small geographic regions, thus limiting the generalizability of their findings.
Objective: To describe the trends in the prevalence, management, and resource utilization for perinatal PTX in the United States.
Design/Methods:
This was a population-based, retrospective cross-sectional analysis of newborn hospitalizations with gestational age (GA) ≥35 weeks within the National Inpatient Sample (NIS) from 2016-2020. The NIS was queried using the ICD-10 CM diagnosis code, P25.1, to identify all neonatal hospitalizations with a diagnosis of PTX. ICD procedure codes were used to identify those who had CT. The outcomes of interest were the trends in CT, resource utilization, and its predictors. Cochran-Armitage and Jonckheere-Terpstra trend tests were used for trend analysis of categorical and continuous variables, respectively. Predictors of length of stay (LOS) and cost were identified using multivariable logistic regression. P-value < 0.05 was considered significant.
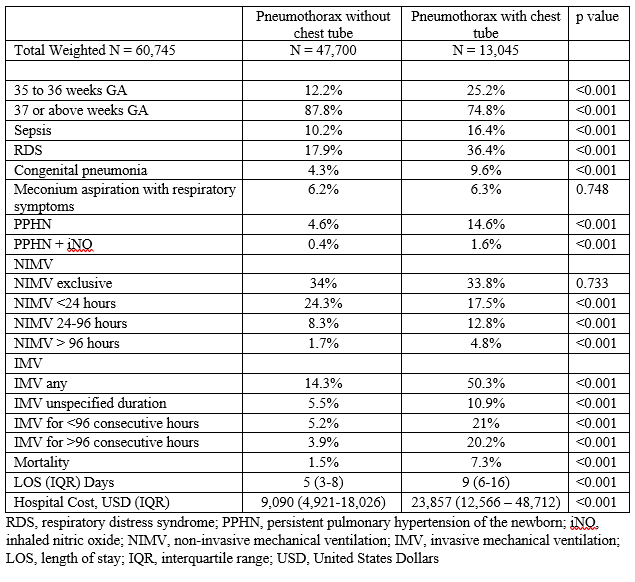
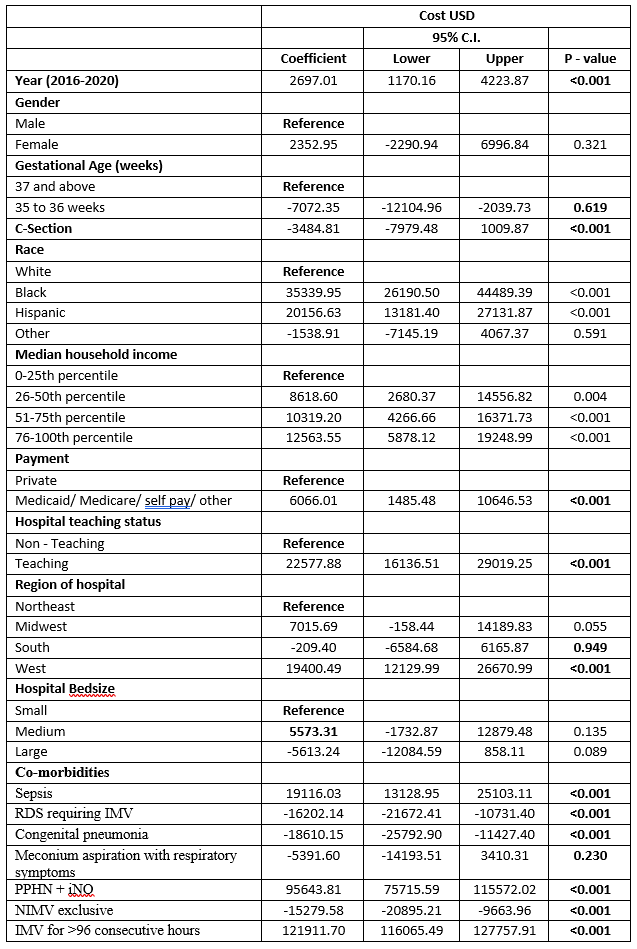
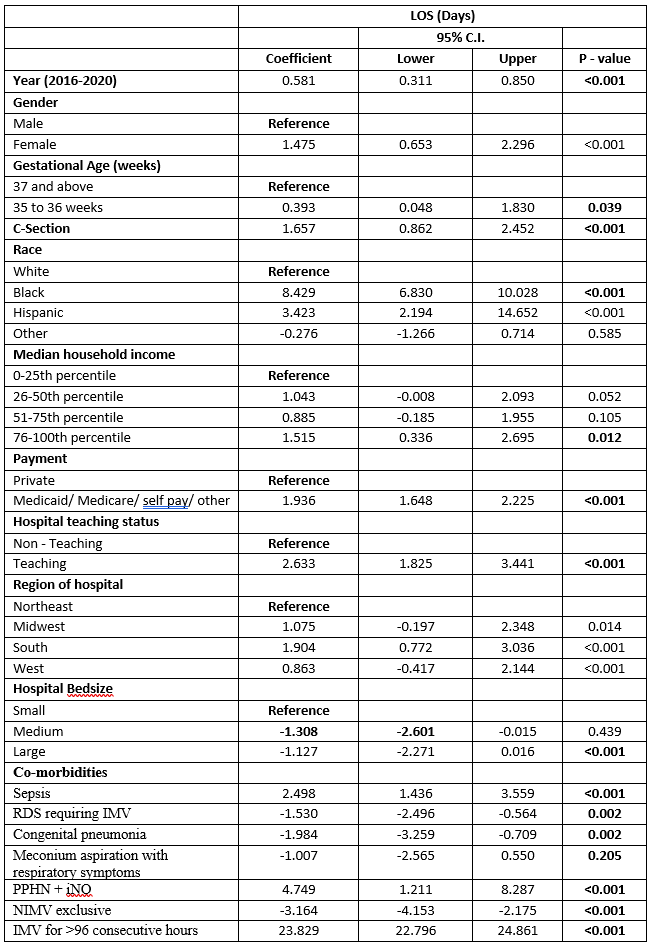
Results: Among 18.5 million newborns, 60,745 (3.27 per 1,000 live births) had PTX and 13,045 (21.5%) had CT placed. The prevalence of PTX increased from 3.2 per 1,000 live births in 2016 to 3.4 per 1,000 live births in 2022 (Ptrend < 0.001) while the rate of CT placement remained unchanged (20.7% in 2016 to 21.5% in 2020, P<sub>trend = 0.271). Utilization of non-invasive mechanical ventilation (NIMV) increased significantly from 23.4% to 36.7% (Ptrend < 0.001). As shown in Table 1, those with PTX requiring CT were more likely to be preterm, have sepsis, respiratory distress syndrome, congenital pneumonia, persistent pulmonary hypertension of the newborn, and more likely to receive invasive mechanical ventilation (IMV). Further, those with CT were more likely to experience in-hospital mortality than those without (7.3% vs 1.5%, P< 0.001). Among the PTX hospitalization requiring CT placement, neonates who were managed on NIMV exclusively had a significantly lower median length of stay (β=-3.16, 95% CI -4.15, -2.17, p < 0.001) [Table 2] and hospital cost (β=-15279.58, 95% CI, -20895.21, -9663.96, p< 0.001) [Table 3].
Conclusion(s):
There was a significant increase in NIMV use in the management of neonatal hospitalizations with PTX, accompanied by an unchanged CT placement rate. NIMV use decreased the LOS and hospitalization costs and therefore, early identification of those neonates who could be managed on NIMV and mastering the skill of NIMV could potentially decrease resource use in the US.