Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
700 - A Rise in Exhaled Carbon Dioxide During Chest Compressions in a Bradycardic Model of Neonatal Resuscitation Predicts Return of Spontaneous Circulation
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 700
Publication Number: 700.445
Publication Number: 700.445
Mary Divya Kasu, John R. Oishei Children's Hospital, Buffalo, NY, United States; sylvia Gugino, State University of New York at Buffalo, Buffalo, NY, United States; Justin Helman, University at Buffalo, Grand Island, NY, United States; Nicole Bradley, University at Buffalo, Buffalo, NY, United States; Sylvia F. Gugino, State University of New York at Buffalo, Buffalo, NY, United States; Mausma Bawa, Boston Children's Hospital, Brookline, MA, United States; Arun Prasath, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Clariss Blanco, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Hamza F.. Abbasi, University at Buffalo, east amherst, NY, United States; Munmun Rawat, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Praveen Chandrasekharan, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States
- MK
Mary Divya Kasu, MD (she/her/hers)
Fellow
John R. Oishei Children's Hospital
Buffalo, New York, United States
Presenting Author(s)
Background: In neonates requiring chest compression (CC) for bradycardia during resuscitation, there is no evidence to support the use of a respiratory monitor that measures exhaled carbon dioxide (EtCO2) to determine the effectiveness of CC or return of spontaneous circulation.
(ROSC). Although an electrocardiogram (EKG) is the best tool to assess heart rate (HR), during CC, it may not be reliable. No studies so far have evaluated the use of EtCO2 as a feedback device during CC and predicted ROSC in a bradycardic neonatal resuscitation model.
Objective: To evaluate the use of continuous capnography during resuscitation of a neonatal bradycardia model of resuscitation.
Design/Methods: Persistent bradycardia is induced by umbilical cord occlusion in 16 near-term ovine models (139-142d gestation) and resuscitated as per NRP guidelines. ETCO2, invasive systolic blood pressure (SBP), heart rate (HR), and carotid blood flow (CBF)
were continuously monitored. Preductal arterial blood gases were obtained every min. Resuscitation was continued to ROSC or
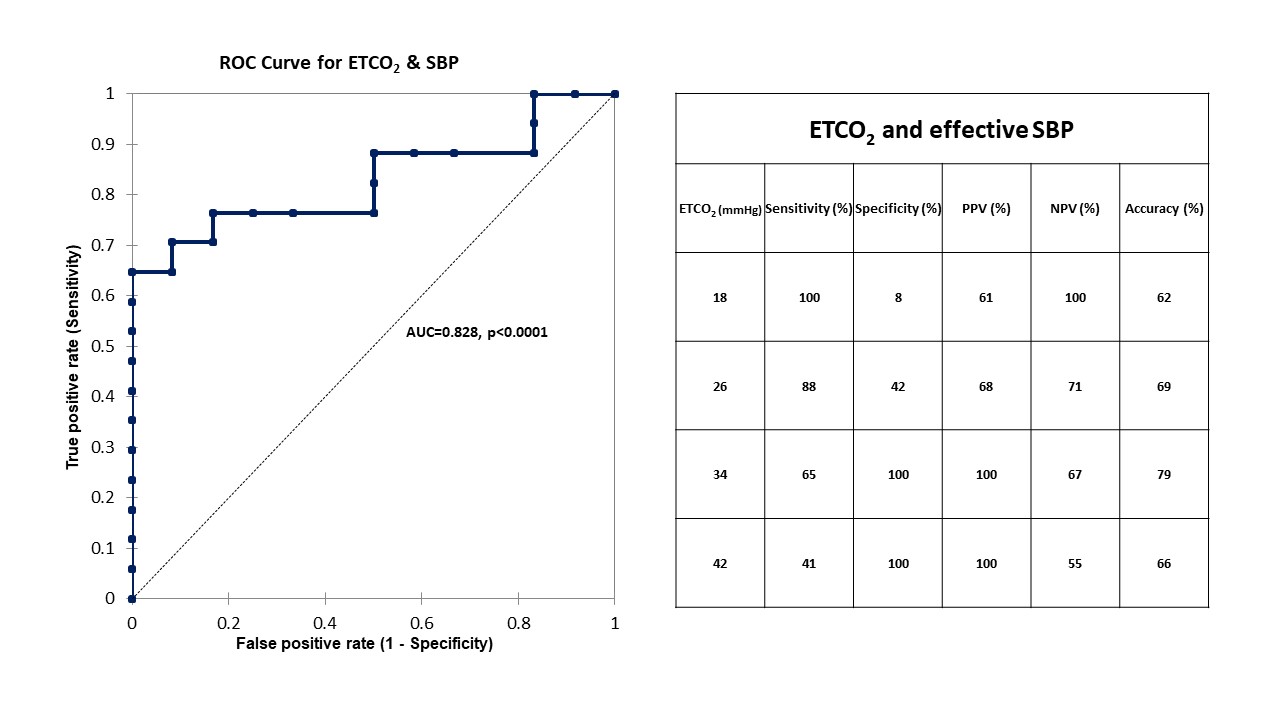
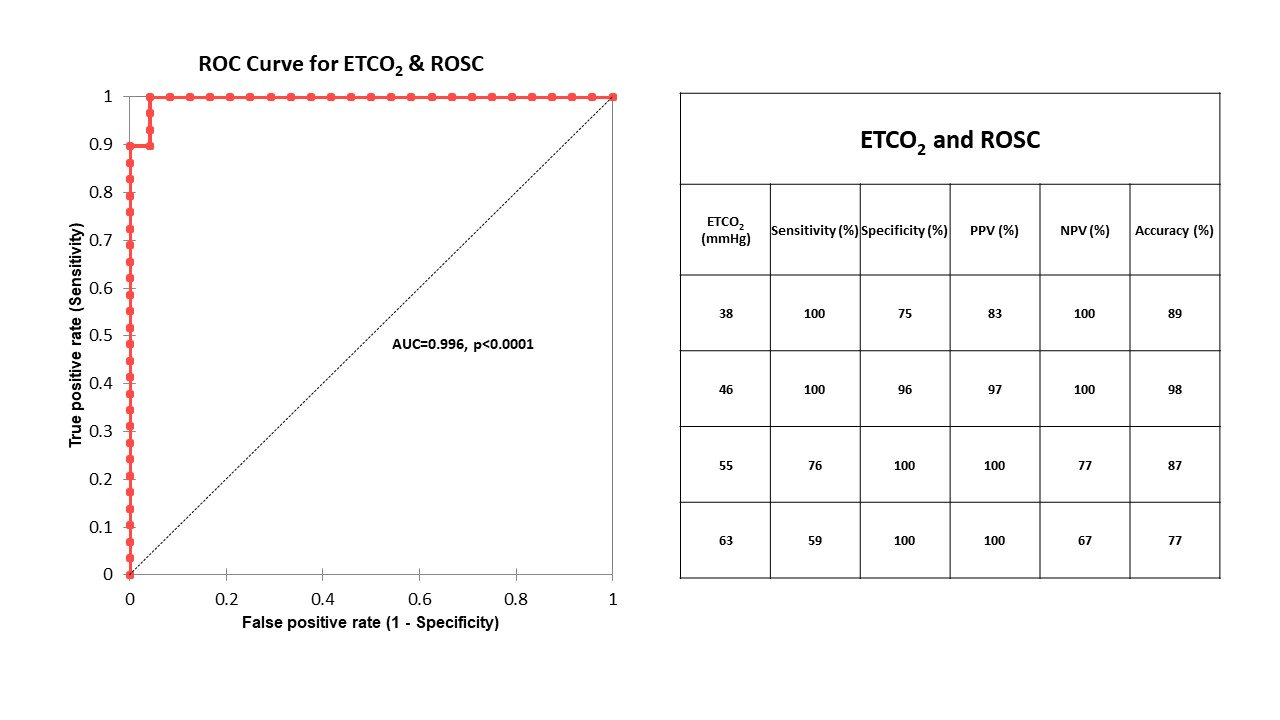
until 20 min after birth. Effective SBP during CC was empirically defined as CC generating a SBP > 50% of baseline. ETCO2 threshold for SBP >50% baseline and ROSC were determined. True positives were plotted against false positives for different test cut-off points under the ROC (receiver operator curve). The cut-off points were assessed based on the area under the curve (AUC), accuracy, and the best sensitivity/specificity.
Results: Out of the 16 lambs with bradycardia, 12 achieved ROSC after resuscitation with positive pressure ventilation (PPV), and CC with or without epinephrine (EPI). It took 3.5±1.5 min to achieve ROSC in this transitional bradycardia model. During resuscitation, ETCO2 predicted SPB ≥ 30 (~50% greater than baseline) mmHg during CC (AUC - 0.828, p< 0.0001) (figure1). At ROSC, ETCO2 increased from 27.7±12 mmHg to 68±17 mmHg (p< 0.0001). ETCO2 predicted ROSC (AUC - 0.996, p< 0.0001) (figure 2). EtCO2 value of 46 had 100% sensitivity and 96% specificity in predicting ROSC.
Conclusion(s): In a large transitional bradycardic neonatal resuscitation model of perinatal asphyxia, continuous ETCO2 monitoring was helpful in determining effective SBP during CC before ROSC. ROSC was associated with a rapid increase in ETCO2. Our translational study supports the use of the respiratory monitor and using ETCO2 data as a predictor for effective CC and ROSC while CC are performed for bradycardia during neonatal resuscitation.