Neonatal Quality Improvement
Neonatal Quality Improvement 7
218 - Improving the Safety of Furosemide Treatment for Chronic Lung Disease in NICU
Publication Number: 218.441
- CT
Christie M. Traynor, NNP-BC (she/her/hers)
Neonatal Nurse Practitioner
Cohen Children's Medical Center
New Hyde park, New York, United States
Presenting Author(s)
Background:
Diuretics are frequently used in the NICU to treat infants with chronic lung disease. Short term improvements in respiratory parameters may be seen in response to loop diuretics such as furosemide, but pharmacologic tolerance often abrogates long-term benefit. Therefore, the use of furosemide for chronic lung disease in infants is controversial. Potential adverse effects include electrolyte abnormalities and bone demineralization.
Objective:
Our goal was to improve the safety of furosemide use for lung disease in our NICU by 1) limiting patient selection to only those at highest risk for chronic disease, 2) defining duration of exposure, 3) instituting standard electrolyte monitoring to minimize toxicity, and 4) reducing the use of repeated trials of furosemide for infants with no response to an initial trial.
Design/Methods:
We instituted a practice bundle for chronic lung disease in preterm infants (< 32 weeks GA), and instruction for providers began in Jan 2021. Furosemide may be used at providers’ discretion, with no specific indications provided. Bundle elements to improve the safety of furosemide include: 1) initial course only if requiring positive end-expiratory pressure (not low-flow nasal cannula), 2) initial course < 5 days with transition to thiazides if effective, 3) monitoring electrolytes at least once during the course, and 4) repeat course only if measurable benefit, defined as decrease in MAP by > 2 cm H20 or FiO2 by > 2%, or transition to a less invasive mode of respiratory support. Bundle reliability was assessed from Jan 2021-Oct 2022 (n = 45).
Results:
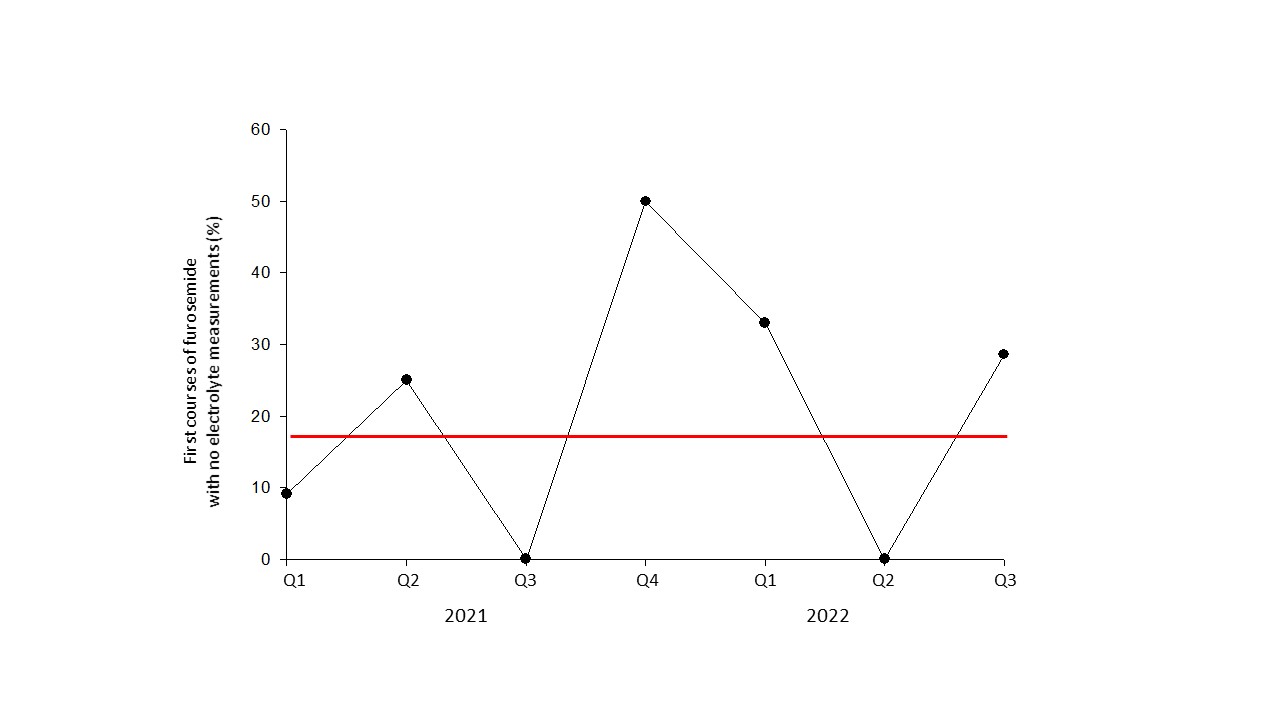
No infants received furosemide while on low-flow nasal cannula after Sept 2021 (Fig. 1). Duration of initial courses of furosemide decreased from > 5 days to 2 days by Oct 2021 (Fig 2). However, surveillance of electrolytes did not improve, with 18% of initial courses without any measurements (Fig. 3). Although 62% of initial furosemide courses had measurable short-term benefit, only 59% of the 17 infants receiving second courses had shown any response to their first course. The incidence of BPD and NICU length of stay did not change.
Conclusion(s):
Standardization of patient selection and duration of furosemide use in the NICU may improve safety as part of a practice bundle for infants with chronic lung disease. A structured, evidence-based program for providers on the risk-benefit ratio of furosemide for chronic lung disease will likely be needed to improve bundle reliability for monitoring electrolytes and limiting repeat courses. .jpg)
.jpg)