Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 6: Primary & Subspecialty Outpatient QI Group 1
254 - Implementation of Forearm and Wrist Treatment Algorithm Decreases Follow-Up Burden, Improves Office Efficiency, and Decreases Cost
Publication Number: 254.452

Alexandria Rundell, Bachleors (she/her/hers)
Clinical Research Coordinator
Akron Children's Hospital
Medina, Ohio, United States
Trinity K. Samson
MD/PhD Student
Northeast Ohio Medical University
Lakewood, Ohio, United States
Presenting Author(s)
Co-Author(s)
Background:
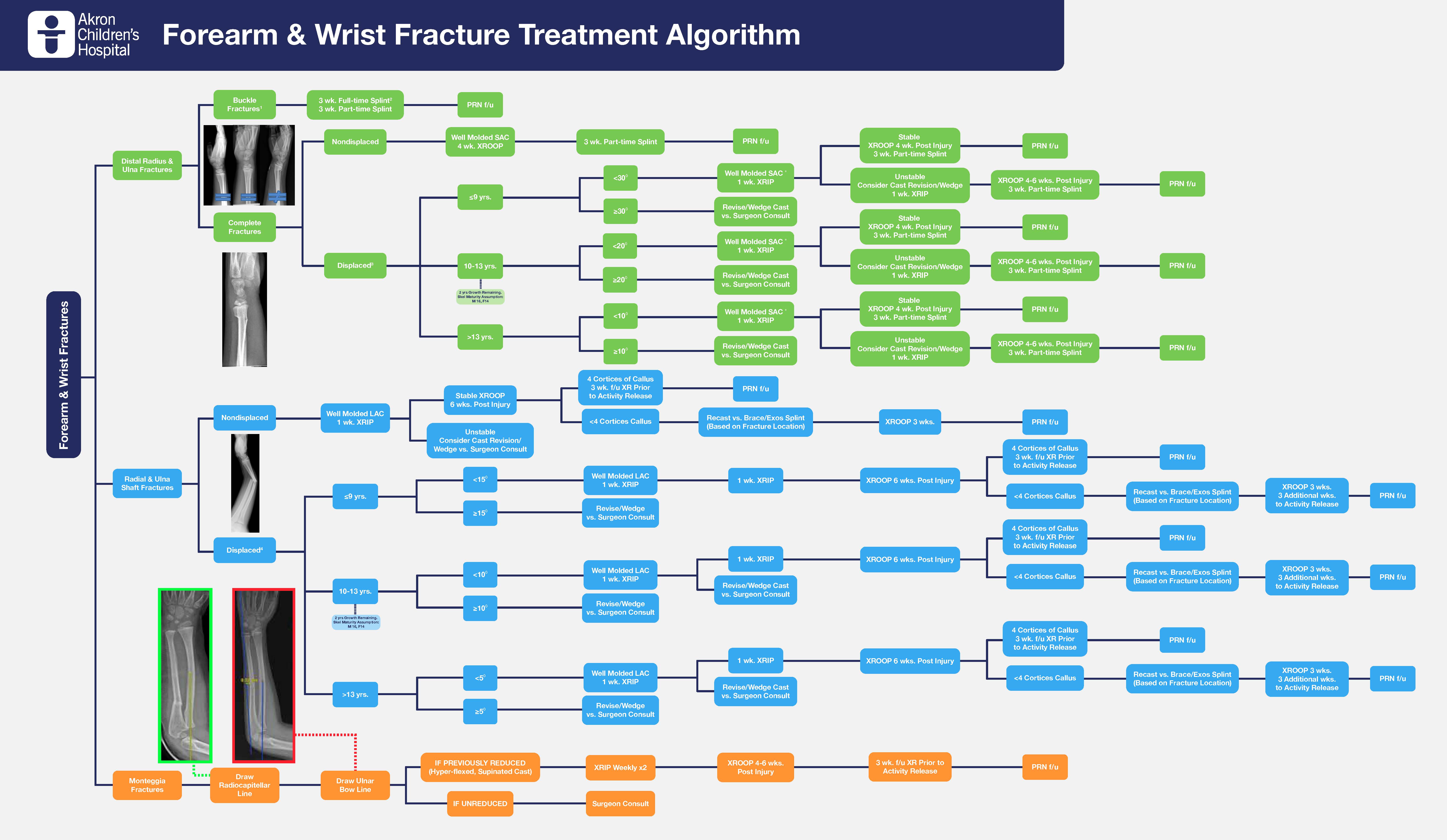
A large pediatric orthopaedic surgical department recognized significant heterogeneity in ambulatory treatment of pediatric wrist and forearm fractures amongst its 22 FTE provider team of surgeons and advanced practice providers. Accordingly, an evidenced based comprehensive treatment algorithm was created and implemented to standardize care (Figure 1).
Objective: We seek to investigate clinical outcomes and cost of treatment prior to and following the implementation of the Forearm and Wrist Fracture Treatment Algorithm.
Design/Methods:
This is a single institution retrospective review of pediatric patients who underwent treatment for forearm and wrist fractures during the traditional regional trauma season prior to the implementation, May through October 2019, and following implementation of the algorithm, May through October 2021. Patients ≤18 years with a forearm or wrist fracture of the radius and/or ulna were identified from an electronic medical record query using ICD-9 and ICD-10 codes. Post-implementation outcomes were compared between patients receiving algorithm-compliant treatment and those who did not using the same methodology.
Results:
1,261 patients were included (614 pre-algorithm, 647 post-algorithm), without differences between cohorts in sex, ethnicity, race, age, fracture type or laterality. 76% of treatment complied with algorithm recommendations following implementation, contributing to significant increase in brace use without casting (2.6% vs 5.4%, p=0.012), decrease in the number of cases that required revision of treatment plan (13.7% vs 7.6%, p=0.001) or cast adjustment (10.4% vs 7.7%, p=0.027), decrease in the length of cast immobilization (37 days vs 35 days, p=0.004), decrease in number of follow up visits (2 visits vs 1 visit, p< 0.001), and decrease in number of radiographic series obtained (3 series vs 2 series, p< 0.001). A total savings of $304.51 was noted per patient for the 647 patients post algorithm, leading to a $197,017.17 savings to patient/payor overall. These improvements contributed a trend towards higher likelihood of acceptable outcomes and fewer complications. For distal radius fractures, there was a significant increase in complications among patients for whom treatment was not compliant with the algorithm (1.4% vs 6.4%, p=0.042).
Conclusion(s): Implementation of an evidence-based treatment algorithm for common wrist and forearm fractures significantly decreases follow up burden, increases office efficiency, and decreases cost with a trend for improved outcomes and fewer complications.