Quality Improvement/Patient Safety: Subspecialty-specific QI: see specialties above
QI 7: Primary & Subspecialty Outpatient QI Group 2
268 - Improving breastfeeding exclusivity at one community hospital: from good to – almost – great
Publication Number: 268.453

Daniela Hochreiter, MD (she/her/hers)
Associate Professor of Clinical Pediatrics
Yale New Haven Children's Hospital
New Haven, Connecticut, United States
Presenting Author(s)
Background: The Center for Disease Control and Prevention (CDC) estimates national breastfeeding exclusivity in the first week of life at 62%; this drops to 24.9% by 6 months of life. The national Healthy People 2030 (HP2030) program has set national aims to increase 6-month breastfeeding exclusivity from 24.9% to 42% and to decrease non-medically indicated formula supplementation in the first two days of life from 19.4% to less than 14.2%. Community hospital births account for nearly 40% of all deliveries nationally and thus are a significant target for breastfeeding improvement.
Objective:
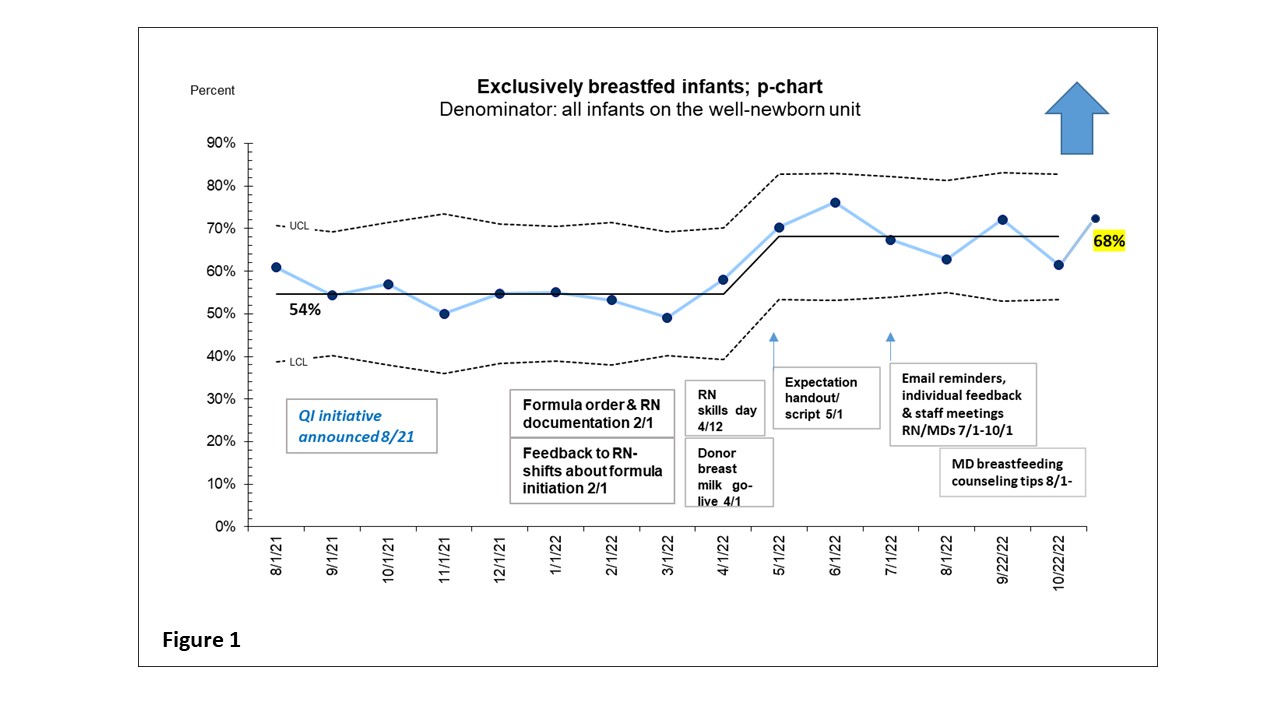
Through quality improvement (QI) methodology, we aimed to increase breastfeeding exclusivity from 54.7% to 65% in infants at one tertiary care affiliated community hospital well-newborn unit over 1-year (8/2021 – 8/2022). Our secondary goal was to decrease non-medically indicated formula supplementation from 28% to less than 20%.
Design/Methods:
We collected baseline data over 6 months through retrospective chart review. A multidisciplinary team of nurses, lactation consultants, midwives, and hospitalists was formed. Plan-do-study act cycles centered around increasing staff engagement through lactation licensure (e.g. CLC and IBCLC training) and accountability through enhanced documentation of lactation-specific conversations with mothers, standardization of teaching scripts, creation of a donor breast milk program, staff feedback, lactation skills days for nurses and tips for hospitalists.
Results: We included at total of 878 infants (430 during the baseline period). Special cause was achieved by 5/1/22 with a center line shift from 54.7% to 68%, which has been sustained for least 6 months (Figure 1). “Fear of not having enough milk” was the most common barrier to breastfeeding exclusivity. Formula supplementation was predominantly initiated on night-shift. Rational subgrouping showed that Hispanic mothers had a higher percentage of non-medically indicated formula usage. Our secondary goal showed a down-ward trend but did not meet special cause. Nursing shortages negatively impacted time spent on counseling.
Conclusion(s):
At one community hospital, a QI team improved exclusive breastfeeding at discharge by over 10% and well above the national 7-day average of 62% demonstrating that the transition from good to – almost – great is feasible. Key interventions focused on staff engagement, accountability, official lactation licensure and the initiation of a donor breast milk program in the well-newborn unit. The next step will be outreach to community obstetric practices to enhance prenatal maternal counseling.