Neonatal Pulmonology
Neonatal Pulmonology 5: NICU Practices
147 - Perinatal Pneumothorax: Regional Variation in Prevalence, Hospital Course, Outcomes, and Resource Use in the United States
Publication Number: 147.437
- HD
Harshit Doshi, MD
Attending Neonatologist
Pediatrix Medical Group of Florida
Venice, Florida, United States
Presenting Author(s)
Background:
Pneumothorax (PTX), which occurs in 1-2% of term infants, is a significant cause of morbidity. Geographic variation in the incidence and management of PTX has been observed but not previously investigated in detail.
Objective:
To compare hospital course, outcomes, and care practices of newborn hospitalizations with PTX in the different census regions of the United States (US).
Design/Methods:
This was a population-based, retrospective cross-sectional analysis of newborn hospitalizations with gestational age (GA) ≥35 weeks within the National Inpatient Sample (NIS) from 2016-2020. The NIS was queried using the ICD-10 CM code P25.1 to identify all neonatal hospitalizations with a diagnosis of PTX. ICD codes were used to identify associated comorbidities and procedures. The outcomes of interest were the geographic differences in the prevalence, outcomes, and resource use (length of stay-LOS, and cost) for perinatal PTX. The US was stratified into 4 regions (Northeast, Midwest, South, and West) according to the US Census Bureau data. Differences were assessed using a chi-square test and multivariable logistic regression analysis as appropriate. P-value < 0.05 was considered significant.
Results:
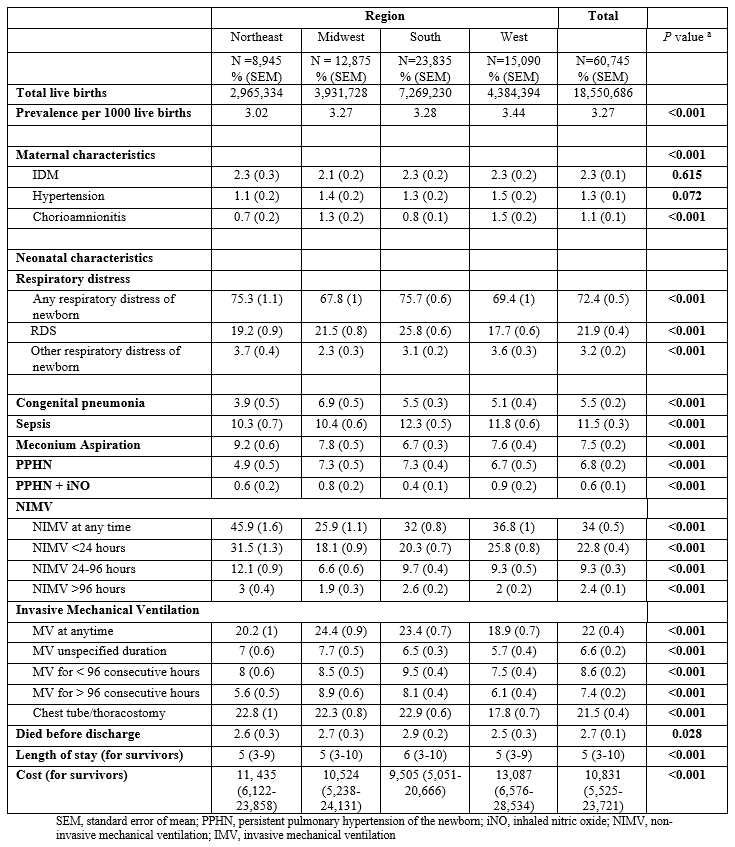
Among 18.5 million newborns born at ≥35 weeks GA, 60,745 (3.27 per 1,000 live births) had PTX. Characteristics of the study population: males 68.75%, Cesarean delivery 31.8%, white race 55%, Medicaid 50.3%, and 82.4% admitted to teaching hospitals. The prevalence of PTX (per 1000 live births) varied from 3.02 in the Northeast to 3.44 in the West (P< 0.001). There were significant differences in associated co-morbidities such as chorioamnionitis, respiratory distress syndrome, congenital pneumonia, invasive mechanical ventilation, non-invasive mechanical ventilation, and chest tube placement across the geographic regions (table 1). The West region was associated with decreased odds of death (odds ratio (OR) 0.75; 95% confidence interval (CI): 0.62-0.9) when compared to the Northeast. Similarly, the West region was associated with increased hospital cost (β=$9,315, 95% CI: $6,663-12,076). Compared to the Northeast, the Midwest (β=0.92 days, 95% CI: 0.47-1.38 days), the South (β=1.82 days, 95% CI: 1.41-2.23 days), and the West (β=0.95 days, 95% CI: 0.51-1.34 days) were associated with increased LOS.
Conclusion(s):
The prevalence, outcomes, and resource use varied across different hospital regions for newborns with perinatal PTX. Regional variation should be studied further to determine benchmarking standards and enhance quality improvement and resource utilization projects related to PTX.