Neonatal General
Neonatal General 10: Outcomes
62 - Length of hospital stays in preterm infants according to gestational age and birth weight: a national benchmark.
Publication Number: 62.429

ibrahim Qattea, MD (he/him/his)
Fellow
Nassau University Medical center
East Meady, New York, United States
Presenting Author(s)
Background:
Preterm births occur in >10% of all pregnancies with a national cost of $25.2 billion ($64,815 per preterm birth). Almost $17.1 billion ($44,116 per preterm birth) of the cost is attributed to daily routine hospital charges. However, the length of hospital stay (LOS) has not been studied in preterm populations.
Objective: To establish national benchmarks for LOS in surviving preterm infants stratified by gestational age (GA) and birth weight (BW) categories.
Design/Methods:
We used de-identified patient data from the Healthcare Cost and Utilization Project (HCUP) from the Agency for Healthcare Research and Quality (AHRQ) for 2016-2020. All infants with a documented GA at 23- 36 weeks were included in the study.
Results:
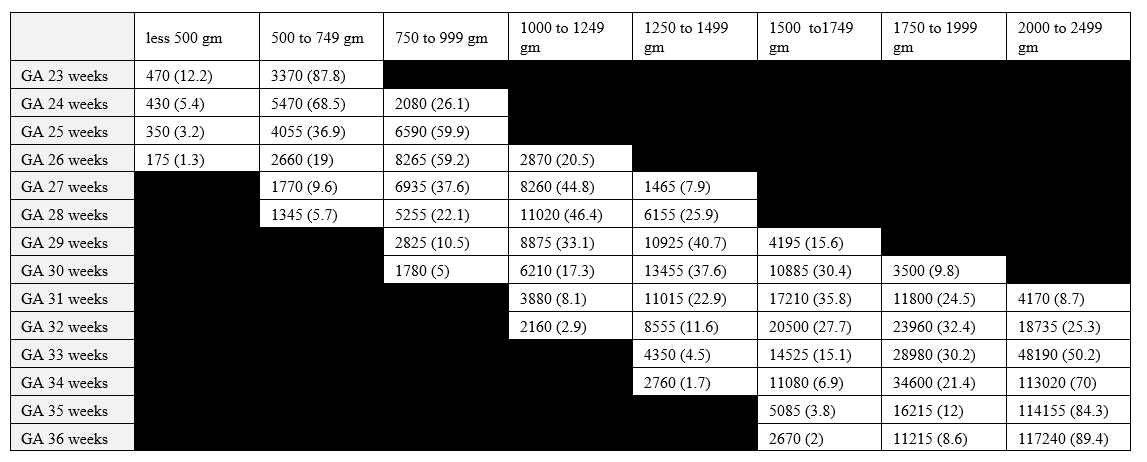
We identified 18,905,605 infants (9,503,450 males and 9,036,791 females) born during the study period. Infants who died or were transferred to another facility were excluded. Among the 18,540,240 included infants, 1,812,329 infants were preterm < 36 weeks and alive. The number and percentage of preterm infants in each GA are presented in Table 1.
Infants born with GA of 23 weeks have LOS of 130-132 days. All infants born at 23-26 weeks have LOS >100 days. Within each GA, BW categories impacted LOS significantly. The mean length of stay of preterm infants according to GA and BW categories are presented in Table 2.
Conclusion(s): The mean LOS is affected by the BW category, in addition to GA. The provided benchmark values can be useful for neonatal units when counseling parents and when structuring quality improvement projects aimed at decreasing LOS.
.png)
