General Pediatrics: Primary Care/Prevention
General Pediatrics 7
302 - Evaluating Effective Partnerships Between a Pediatric Mobile Medical Program and Community Organizations
Publication Number: 302.408

Hope E. Rhodes, MD. MPH (she/her/hers)
General Pediatrician
Children's National Health System
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Children’s National Mobile Medical Program (CNH MMP) has provided a variety of primary care services throughout the District of Columbia for over 20 years. During the COVID-19 pandemic, the MMP leveraged its expertise in placed-based care by forming community partnerships with public/charter schools, development centers and Health Maintenance Organizations to increase access to care. The CNH grew rapidly from 2020-2022, forming several new partnerships to conduct well child visits, sports physicals, immunization drives and social determinants of health screenings across the DC and Prince George’s County, MD.
Objective: 1. Describe community partners: location, target patient population, services rendered.
2. Review community partners' data from the Partnership Assessment Tool for Health Questionnaire.
Design/Methods:
The PATH questionnaire is designed to maximize the impact of healthcare organizations’ partnerships with community organizations. The survey tool was distributed to 20 organizations. Each organization was asked to rate their partnership with the mobile medical program in the following domains: internal/external relationships, service delivery and workflow, funding and finance, data and outcomes. Community partners with the lowest and highest assessments will be invited to participate in virtual semi-structured interviews to provide more key themes and sub-themes.
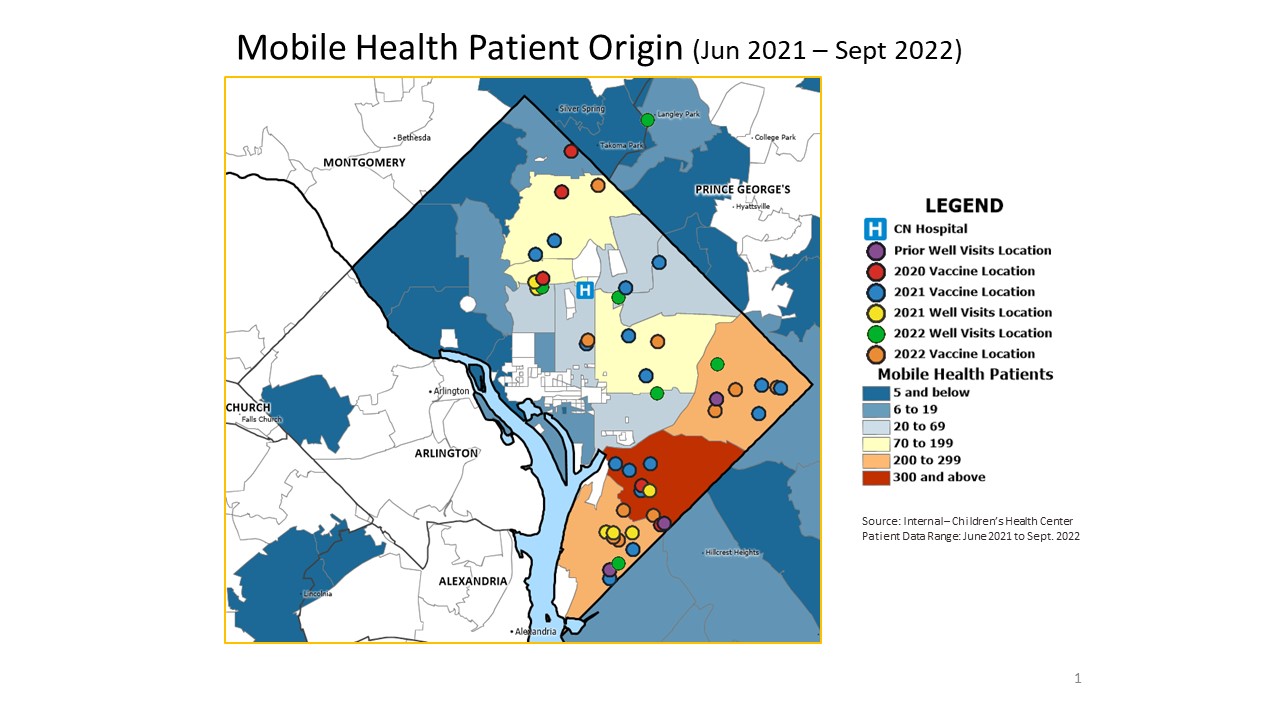
Addresses for each of the community organizations were used to map the distribution of neighborhoods serviced by the mobile program.
https://www.chcs.org/media/Partnership-Assessment-Tool-for-Health_-FINAL.pdf
Results: The CNH MMP has tripled the number of community partners during the pandemic, partnering with over 30 schools and organizations. The community’s reception of the CNH MMP has been largely positive with several requests for additional services. Community organizations have highlighted the importance of improving the following: workflows during the date of service, capacity to accommodate more patients, increased flexibility for walk-ups, and streamlining/reducing registration paperwork. We anticipate that semi-structured interviews will further elucidate areas to improve communication, service delivery and workflows.
Conclusion(s):
Leveraging community partnerships is a critical step in bridging gaps in care. In addition to the primary care medical home, community partners are a trusted source for parents and families. Community partner feedback is critical and informs ongoing care delivery as we venture beyond the pandemic.