Neonatal Neurology: Pre-Clinical Research
Neonatal Neurology 7: Preclinical 1
3 - Hypothermia enhances behavioral neuroprotection by neural stem cells following perinatal hypoxic-ischemic injury without decreasing lesion volume
Publication Number: 3.433
Tommy R. Wood, MD, PhD (he/him/his)
Research Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background:
Perinatal hypoxic ischemic encephalopathy (HIE) is a leading cause of morbidity and mortality, occurring in 0.5-1.5/1000 live births in high resource countries. The only current evidence-based treatment for HIE is whole-body hypothermia (HT). In the Vannucci rat pup model of HIE, human neural stem cell (hNSC) therapy reduces brain injury leading to improved outcomes; however, the effect of HT on hNSCs in vivo remains unknown.
Objective: Evaluate the effect of HT on hNSCs in vivo.
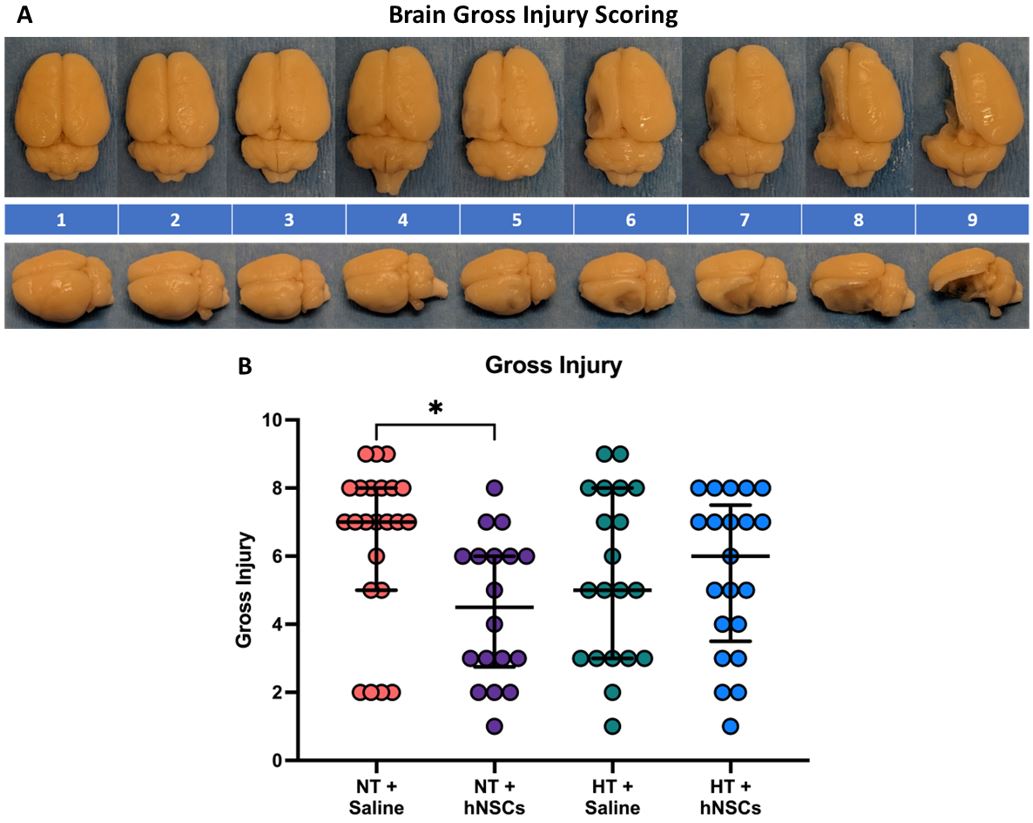
Design/Methods: Term-equivalent (postnatal day 10) rat pups underwent unilateral left common carotid artery ligation followed by hypoxia to induce hypoxic-ischemic brain injury. Within 6hrs, pups were randomized to normothermia (NT) or HT (rectal temperature 33.0°C) for an additional 6hrs. Pups were then randomized to contralateral intraventricular instillation of 10µl of either saline or an hNSC suspension (5x104 cells/µl) 72h after injury. Gross brain injury (Fig. 1A) and Open Field behavior 1 month after injury were evaluated. Outcomes in treated groups were compared to the NT + Saline group with a Kruskal-Wallis test followed by Dunn’s post hoc test.
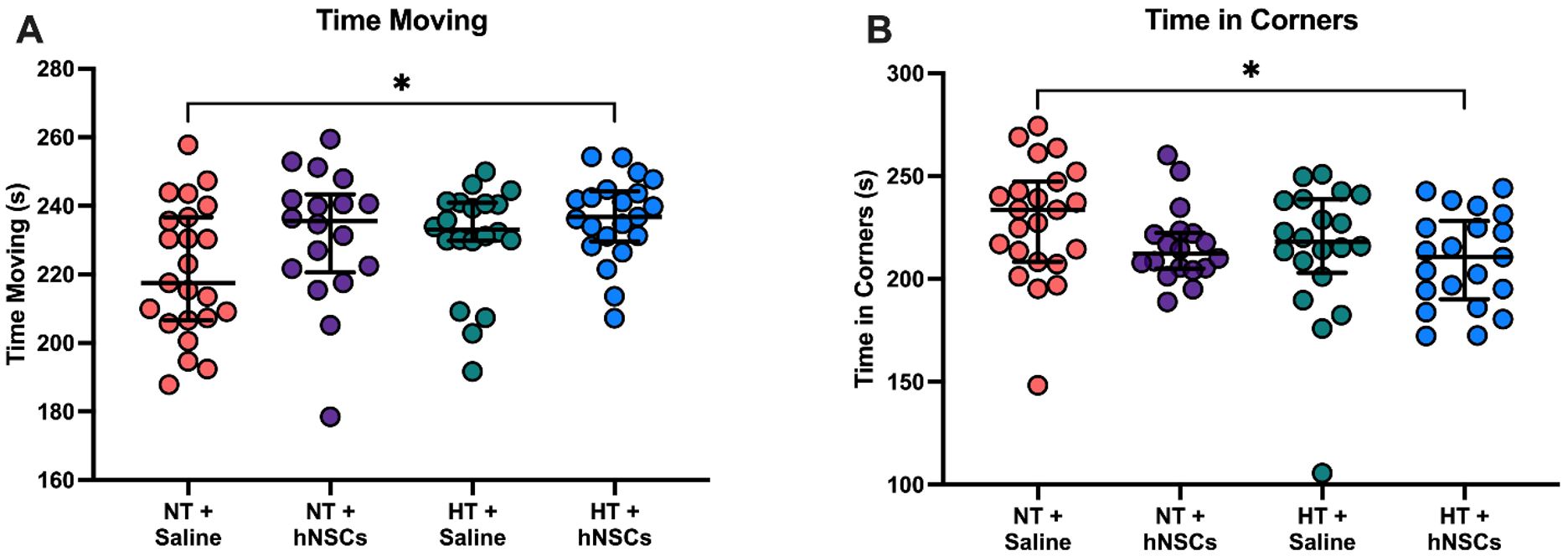
Results: 89 of 108 pups survived surgery and hypoxia. An additional 7 rats were euthanized prior to behavioral testing and sacrifice – 6 for >20% weight loss (4 in the NT+Saline group, 2 in the HT+Saline group), and 1 for poor skin healing following saline infusion (NT+Saline group) – for 82 rats included in this analysis: n=23 NT+Saline, n=18 NT+hNSCs, n=20 HT+Saline, and n=21 HT+hNSCs. Relative to the NT+Saline group, median gross injury scores were non-significantly decreased with any combination of hNSC and/or HT therapy; however, only NT+hNSCs resulted in significantly lower injury scores (p=0.016, Fig. 1B). Similarly, while hNSCs and/or HT non-significantly increased median moving time and reduced median time spent in the corners of the Open Field, only rats treated with HT+hNSCs spent significantly more time moving and less time in the corners (p=0.036 and p=0.019, respectively, Fig. 2A-B).
Conclusion(s):
While animals treated with hNSCs and/or HT following experimental HIE show a trend toward improved outcomes, the effect of hNSCs appears to be modulated by prior HT; gross brain injury protection was diminished by the addition of HT yet exploration and anxiety were improved. These results not only support the utility of hNSCs as a potential therapy for HIE with careful investigation in combination with HT, but they also suggest that behavioral recovery may entail more than quantifiable gross parenchymal sparing.