Neonatal Quality Improvement
Neonatal Quality Improvement 7
215 - A Quality Improvement Project to Standardize the use of Premedication for Endotracheal Intubation in the NICU
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 215
Publication Number: 215.441
Publication Number: 215.441
Michelle H. Lucena, The Children's Hospital at Montefiore, Verona, NJ, United States; Toshiba Morgan-Joseph, The Children's Hospital at Montefiore, Bronx, NY, United States; Mimi Kim, Albert Einstein College of Medicine, Bronx, NY, United States; Alecia Thompson-Branch, The Children's Hospital at Montefiore, Bronx, NY, United States

Michelle H. Lucena, MD (she/her/hers)
Fellow in Neonatal-Perinatal Medicine
The Children's Hospital at Montefiore
Verona, New Jersey, United States
Presenting Author(s)
Background: Endotracheal intubation is frequent in the Neonatal Intensive Care Unit (NICU), but it may result in distress and cardiorespiratory instability. Premedication reduces adverse responses and pain associated with this procedure.
Objective: Smart Aim: Primarily, 80% of patients meeting preselected criteria undergoing endotracheal intubation would receive standardized premedication – opioid analgesic and non-depolarizing muscle relaxant. The secondary aims were reducing intubation attempts, complications associated with intubation, and post-intubation airway sequelae.
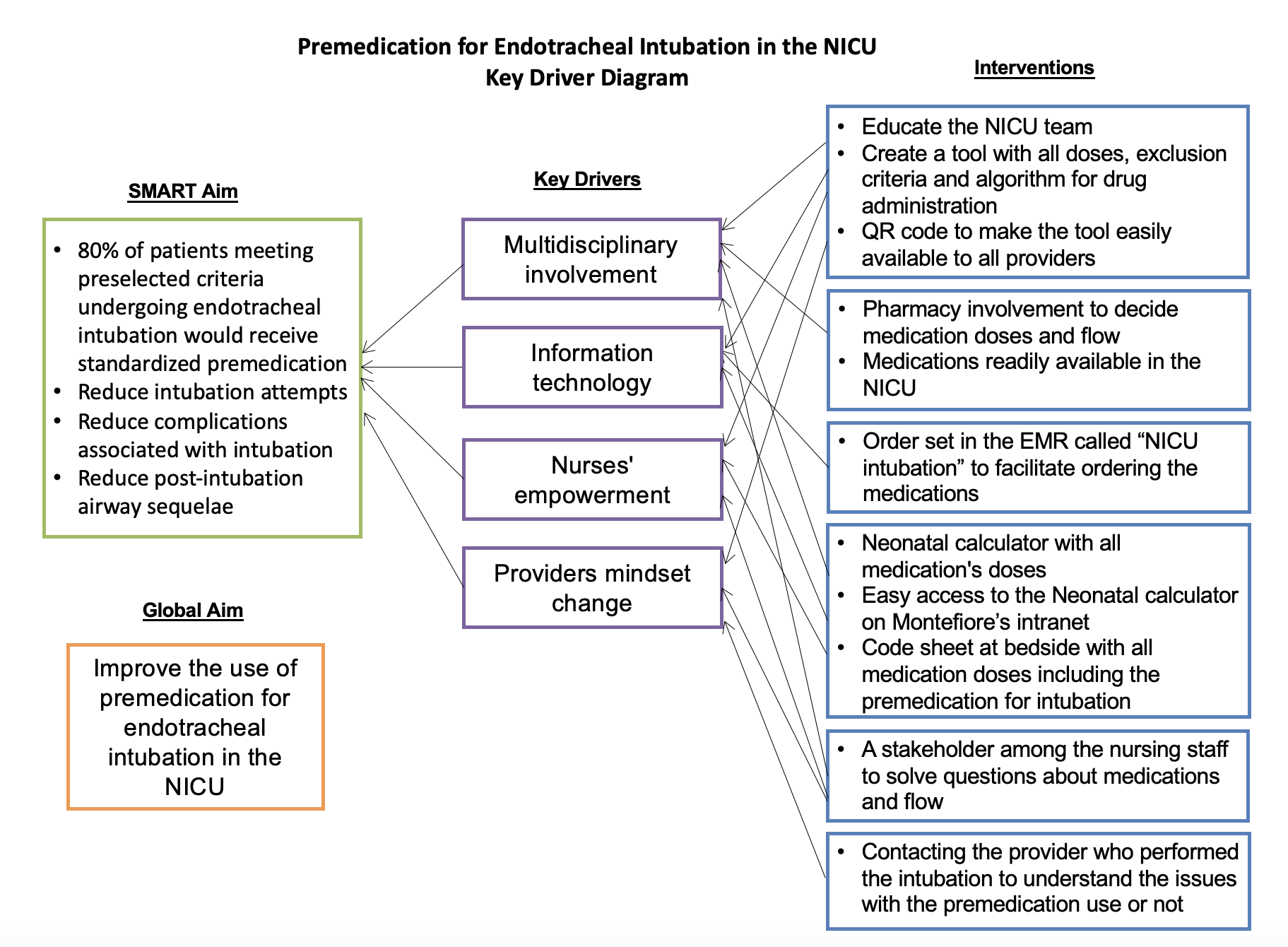
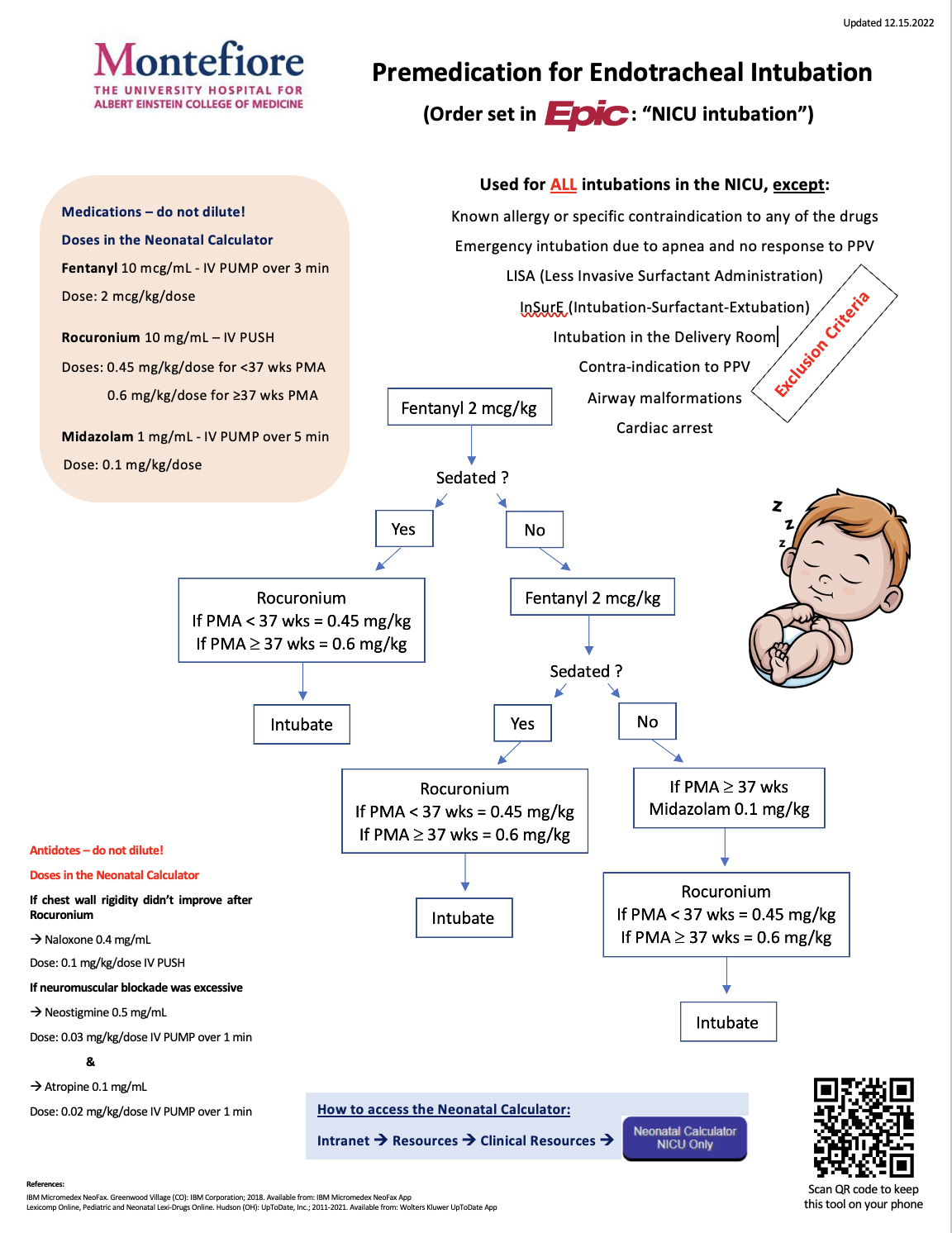
Design/Methods: Measures: Using quality improvement (QI) methodology, we developed a ‘Key diagram’ (Figure 1) for premedication for intubation. Exclusion criteria and medications are shown in Figure 2. Baseline data were collected retrospectively from the electronic medical record (EMR), followed by Plan-Do-Study-Act (PDSA) cycles every 3-4 months and depicted through a statistical processing chart (SPC). Statistical analysis was done utilizing Fisher's exact test to compare categorical variables. Balancing measures included antidotes if chest rigidity was present or if the neuromuscular blockade was excessive.
Results: Between 2021-2022, 98 infants were included in the analysis, with a mean birth weight (BW) of 1282 gm (range: 390 – 5380). The mean postmenstrual age (PMA) was 32.1 weeks (range: 23.3 – 42.6), and the mean postnatal age was 28.6 days (range: 0 – 144). Hypoxemic respiratory failure, the most common indication for intubation, occurred in 44.2% (53/98) of infants. Infants in the premedication group were intubated successfully on the first attempt at a rate of 82.2% (37/45) compared to the non-premedication group, 69.4% (25/36) (p=0.028). The use of premedication over time is shown in Figure 3. Desaturations were not statistically significant between groups, and no airway sequelae were diagnosed. One case of chest rigidity was reported. When the cohort was divided into < 34 wks and ≥34 wks PMA, proportionately, the older infants received more premedication: 72.2% compared to 51.6% in the younger infants (p=0.045).
Conclusion(s): Infants ≥34 weeks PMA received more premedication due to the perception that increased motor activity at this age would prohibit successful intubation. Emerging evidence indicates that increased exposure to painful procedures may lead to poor neurodevelopmental outcomes. Given how common intubation is performed in the NICU, attention to pain control should be paramount. During this QI project period, premedication was associated with successful intubation without an increase in complications.
.png)
