Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 3
684 - Racial and Ethnic Disparities in the Resuscitation and Survival of Periviable Preterm Infants in California
Publication Number: 684.444

Brennan V. Higgins, MD, MPhil (she/her/hers)
Fellow
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: There are well known racial and ethnic disparities in preterm birth and its complications in the United States. However, less is understood about the inequities in periviable birth and the resuscitation and survival of these infants with conflicting and even contradictory results.
Objective: This study seeks to describe rates of active treatment, survival, and morbidity in periviable infants in a recent population-based cohort in California.
Design/Methods:
This retrospective cohort includes infants born between 22 and 25 weeks completed gestation in California between 2011 and 2019. Birth certificates were linked to hospital discharge records and used to obtain demographic, antenatal, perinatal and infant characteristics as well as International Classification of Diseases (ICD) diagnosis and procedure codes. Active resuscitation was defined as survival >1 day or an ICD code for cardiopulmonary resuscitation, intubation, invasive mechanical ventilation, or non-invasive mechanical ventilation. Relative risks were calculated using a saturated race variable so as to compare one racial/ethnic group to all other infants rather than using a White, non-Hispanic reference group.
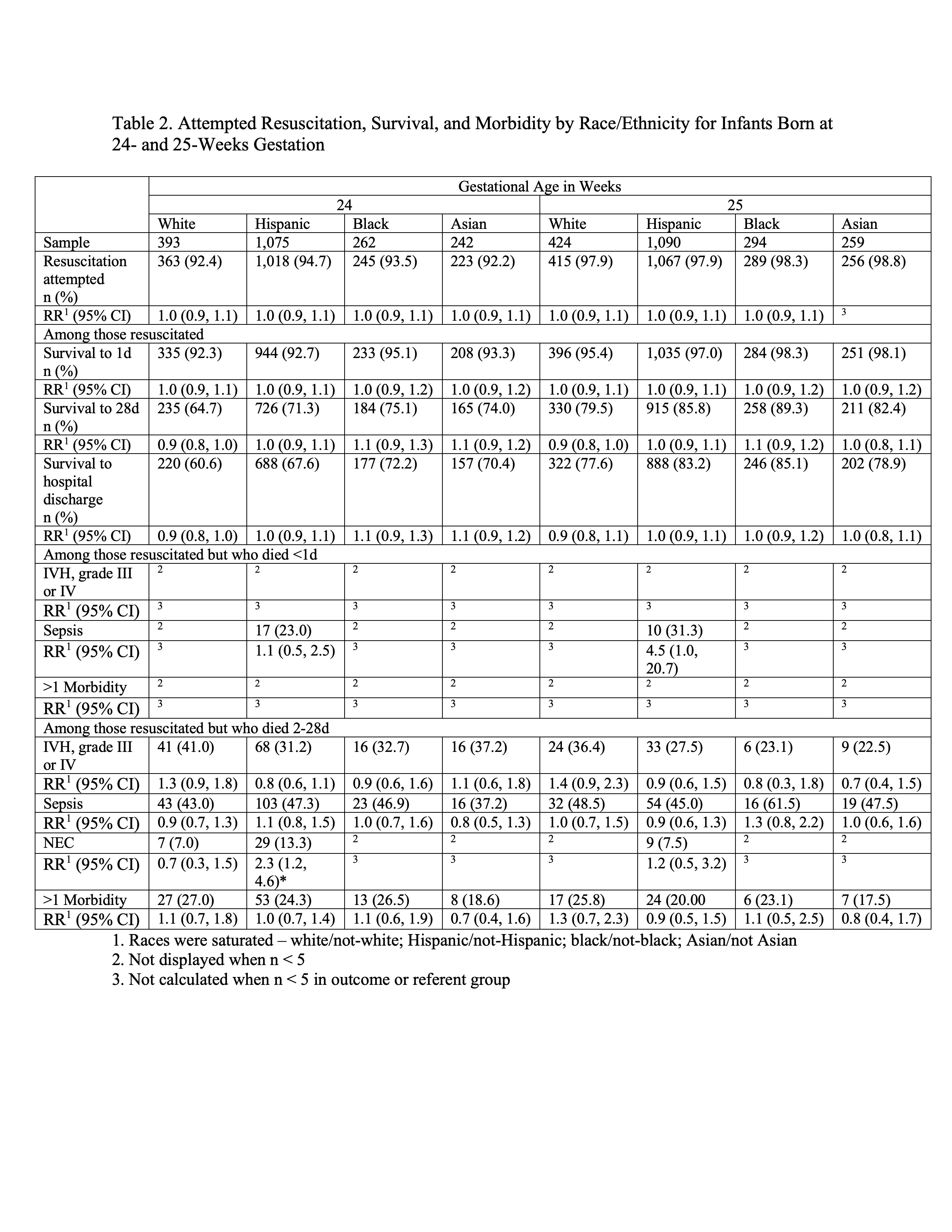
Results: This study includes 7,245 infants born between 22-25 weeks (18% white, 49% Hispanic, 13% black, 11% Asian, 9% other). White infants born at 23 weeks completed gestation were less likely to receive active resuscitation (RR 0.8, 95% CI 0.7-0.97) compared to non-white infants. Additionally, white infants born at 23 weeks who died after resuscitation (between day 2-28) were less likely to have >1 major morbidity (RR 0.5, 95% CI 0.3-0.97) at the time of death. Hispanic infants born at 23 weeks were more likely to receive active resuscitation compared to non-Hispanic infants (RR 1.1, 95% CI 1.002-1.3). There were no differences in rates of active resuscitation by race/ethnicity at 22, 24 and 25 weeks and there were no differences in survival (to 1 day, 28 days, and hospital discharge) after resuscitation across all gestational ages 22-25 weeks.
Conclusion(s):
This study found differences in the provision of active care at 23 weeks completed gestation by race/ethnicity. White infants were less likely to receive active resuscitation and more likely to die with fewer morbidities between day of life 2 and 28 compared to non-white infants. The opposite was seen in Hispanic infants. These patterns highlight the variability in decision making in the face of uncertain outcomes. More research is needed on factors that influence these decisions including periviable counseling and the inequities in this process.
.jpg)