Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 10
592 - Food Insecurity Screening and Intervention Strategies in Pediatric Clinics Across the United States: Opportunities for Innovation
Publication Number: 592.411
.jpg)
Greeshma James, MPH (she/her/hers)
Policy Analyst
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background:
Food insecurity (FI) is associated with poor outcomes for children. While many pediatricians report addressing FI in clinical settings, approaches to integrate FI screening and interventions into practice, and the roles that health systems or alternative payment models (APMs) play in supporting this work has yet to be explored.
Objective:
To describe barriers and facilitators to addressing FI in pediatric clinics, and identify opportunities for practice and policy innovation.
Design/Methods:
This is a mixed-methods study of pediatric practices addressing FI across the US. Participants were recruited via email using snowball sampling. Participants completed an online survey about current FI screening and intervention strategies and practice sociodemographic data. Qualitative interviews were conducted to explore innovative approaches and the role of policies or payment models. Interviews were recorded and transcribed verbatim. Rapid qualitative analysis was used to identify themes.
Results:
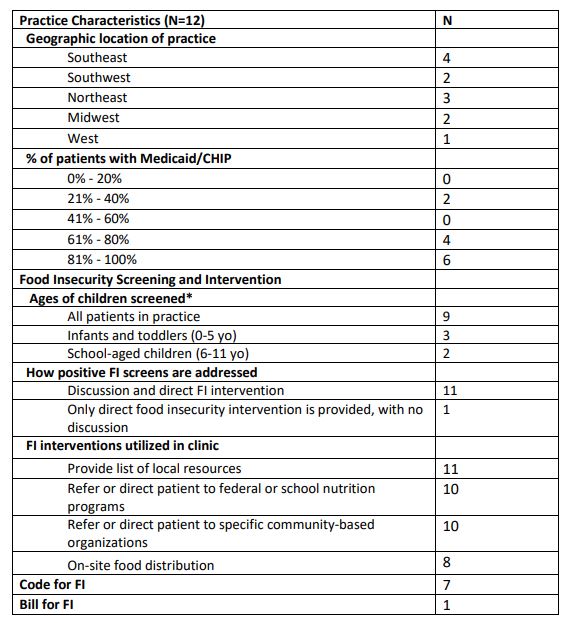
15 pediatricians and 4 care coordinators representing 12 practices were included. Survey results showed that most practices (N=10) served patient populations that were ≥60% Medicaid (Table 1). Nearly all (N=11) provided a food-related resource list to those screening positive and assisted with referrals to federal nutrition programs (N=10).
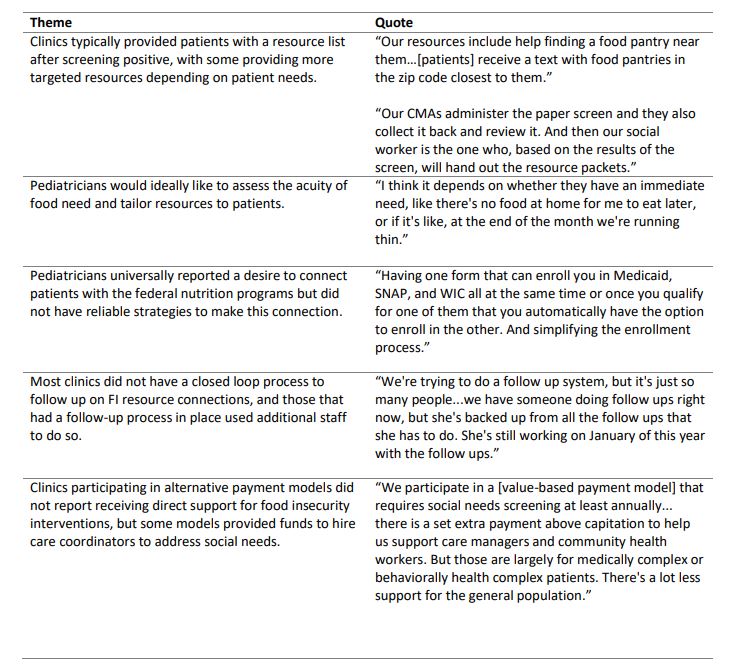
Qualitative analysis revealed 5 main themes (Table 2). (1) Clinics typically provided patients with a resource list after screening positive, with some providing more targeted resources depending on patient needs. (2) Pediatricians would ideally like to assess the acuity of food need and tailor resources to patients. (3) Pediatricians universally reported a desire to connect patients with federal nutrition programs but did not have reliable strategies to make this connection. (4) Most clinics did not have a closed loop system to follow up on FI resource connections. (5) Clinics participating in APMs, which aim to reward high quality care at lower cost and often support programs to address social needs, did not receive direct support for FI interventions. Some APMs provided funds to hire care coordinators to address social needs.
Conclusion(s):
Pediatric clinics use a variety of strategies to address FI but lack standard procedures to ensure needs are met. Designing approaches to integrate federal nutrition programs within clinical settings through data sharing, further leveraging payment models to fund innovative strategies to address social needs, and designing follow up processes for resource connections are important opportunities to address child food insecurity.