Global Neonatal & Children's Health
Global Neonatal & Children's Health 3
533 - Determining Key Practice Indicators of Thermal Management in Nepal Using the Delphi Method
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 533
Publication Number: 533.409
Publication Number: 533.409
Brandon Tomlin, University of Utah School of Medicine, Salt Lake City, UT, United States; Grace Richards, University of Utah School of Medicine, Park City, UT, United States; Bibek Lamichhane, Human Right Peace And Development Forum Nepal, Kathmandu, Bagmati, Nepal; Ranjan Dhungana, Children Medical Mission, Utah, Kathmandu, Bagmati, Nepal; Peter Grubb, University of Utah School of MedicineMD, Salt Lake City, UT, United States; Bernhard Fassl, Northeast Ohio Medical University, Salt Lake City, UT, United States; Allison Judkins, University of Utah School of Medicine, Salt Lake City, UT, United States

Brandon Tomlin, MD (he/him/his)
Physician Fellow, Neonatal-perinatal Medicine
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Neonatal hypothermia is a massive worldwide health burden with a global incidence ranging from 32-85% in hospitals and 11-92% in home births. It has been well studied that neonatal hypothermia is associated with increased morbidity and mortality. Nepal has high rates of hypothermia, with one study in a large hospital finding 43% of their infants were hypothermic. In this hospital, only 4.2% of infants received Kangaroo Mother Care (KMC), an important thermal practice recommended by the World Health Organization (WHO). Another Nepali study estimated 10% of infants at home births receive optimal thermal care. While the WHO practices help prevent hypothermia, due to a lack of resources and cultural practice differences, Nepali physicians may have different priorities for thermal management.
Objective: To identify the key practice standards of thermal management according to Nepali physicians.
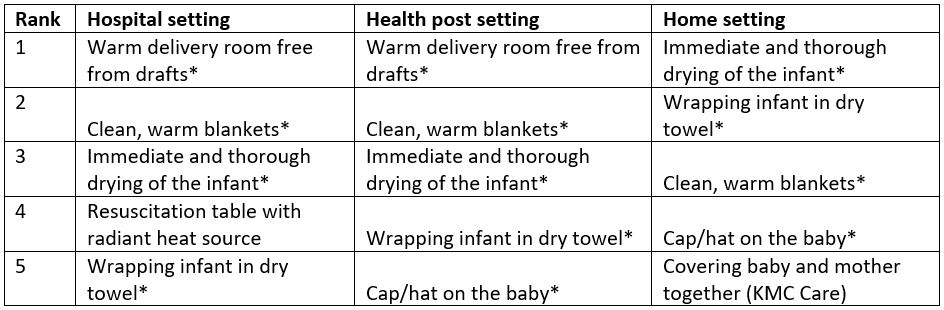
Design/Methods: Our subjects included 6 lead newborn physicians at major birthing centers around the Kathmandu valley. A Delphi process was used to identify the top 5 key practice standards for proper thermal management of the newborn. The process took place over 3 rounds, 1 in person and 2 Qualtrics surveys. 14 practices were identified in the WHO Recommendations on Newborn Health and agreed upon in the 1st in person session. The 14 practices were sorted by rank order of most important for thermal management in three distinct settings: 1)hospital, 2)health post, and 3)home birth. The scores were aggregated and narrowed to 9 practices for the second round and 5 after the final. The results were then sent back to the physicians for comment. Agreement of final ranking was defined as a standard deviation of < 2.25, or < 25% of the range of ranks.
Results: The rank of the top 5 practice standards are shown in Table 1. There was consensus in ranking all aspects except for a radiant heat source in the hospital setting and KMC in the homebirth setting. Comments from the physicians conveyed that those listed were helpful in the immediate delivery phase when the infant is at highest risk, and the most feasible for the setting. Factors such as KMC were deemed not as important because it is used outside of this initial phase, though it is more valued in health posts and homebirths.
Conclusion(s): Nepali physicians view practices that prevent loss of heat immediately after delivery as the key practice indicators for thermal management in all settings, while other practices like KMC are considered less important. This highlights an important area of practice improvement and future implementation studies for neonatal thermal care.