Neonatal General
Neonatal General 10: Outcomes
61 - Machine Learning and Transcriptomics to Predict Respiratory Hospitalization in Very Low Birth Weight Neonates
Publication Number: 61.429

Charles T. Valadie, MD (he/him/his)
Neonatal-Perinatal Medicine Fellow
The University of Texas Health Science Center at San Antonio Joe R. and Teresa Lozano Long School of Medicine
San Antonio, Texas, United States
Presenting Author(s)
Background:
Bronchopulmonary dysplasia (BPD) is a leading cause of morbidity and mortality among premature newborns. The morbidities related to BPD and prematurity put infants and children at risk for additional complications. Identifying neonates at risk for respiratory hospitalization may help reduce healthcare burden.
Objective:
1) Create an early transcriptomic-based prediction model for respiratory hospitalization in very low birth weight neonates (VLBWs).
2) Compare this transcriptomic model to an algorithm built on clinical factors known to associate with long-term respiratory outcomes (e.g., sex, gestational age, BPD definition, oxygen days, 5 minute APGAR).
Design/Methods:
This is a secondary analysis of transcriptomic data derived from 74 very low birth weight neonates (PMID: 24194948). Respiratory hospitalization was defined as an admission secondary to an upper or lower respiratory tract infection that occurred after NICU discharge, but within the first four years of life. Participants were randomly assigned into a training (2/3) and testing cohort (1/3). A random forest machine learning model was built for genes that could serve as optimal predictors for respiratory hospitalization. Using these genes, a generalized linear machine learning model was created to assess their predictive ability in the test cohort.
We then compared the transcriptomic model to a clinical model using the same machine learning approach. Model performance was evaluated using the area under the receiver operating curve (AUC).
Results:
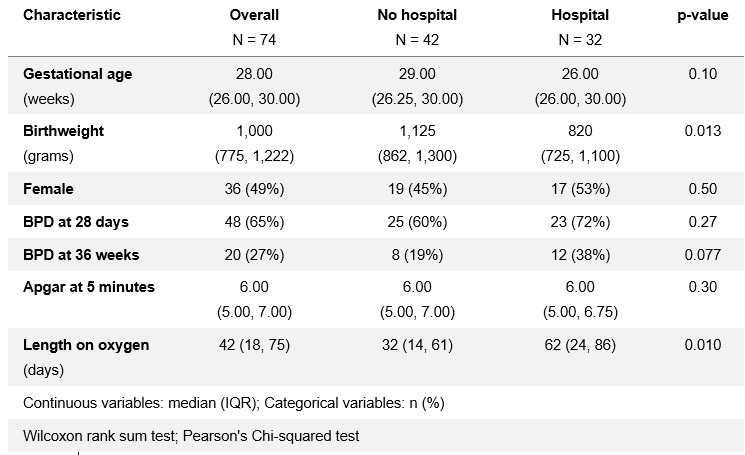
Thirty-two (43.2%) VLBWs had a respiratory hospitalization in the first four years of life. Neonates with a lower birthweight (median weight of 820 grams vs. 1,125 grams, p=0.01) and longer duration of oxygen requirement (median days 62 vs. 32, p=0.01) in the NICU were more likely to be hospitalized. BPD did not associate with respiratory hospitalization.
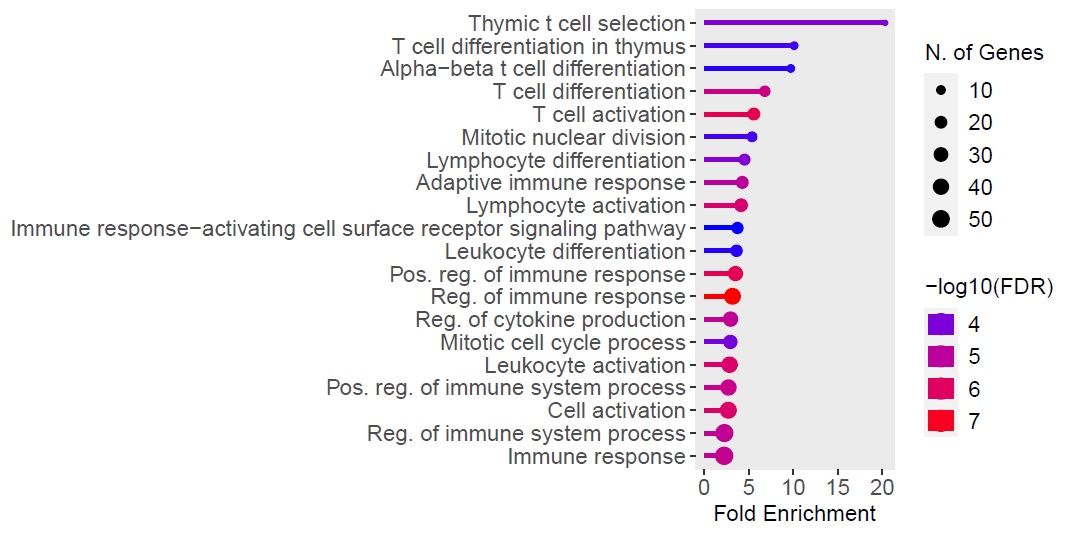
A total of 383 genes were differentially expressed between the groups (false discovery rate < 0.01). The AUC for predicting respiratory hospitalization using birthweight and oxygen days was 94.4% (95% CI, 84.4%-100%), while the AUC using 10 transcripts was 95.1% (95% CI 85.2%-100%). Genes ontologically involved in T cell development differentiated neonates who were later hospitalized.
Conclusion(s):
This study suggests that transcriptomic changes in the first week of life may help in determining which neonates are at higher risk for future respiratory hospitalization. Furthermore, this transcriptomic model performed as well as a model originating from clinical information. Future studies are needed to externally validate our findings..jpg)