Global Neonatal & Children's Health
Global Neonatal & Children's Health 3
544 - Disparities in risk factors for mortality between inborns and outborns at a regional neonatal intensive care unit (NICU) in the Dominican Republic
Publication Number: 544.409

Henna Shaikh, MD (she/her/hers)
Pediatric Global Health Fellow
Children's Hospital of Philadelphia
Seattle, Washington, United States
Presenting Author(s)
Background:
The Dominican Republic (DR) is a low to middle income country (LMIC) with a neonatal mortality rate of 19 per 1,000, above Sustainable Development Goal 3.2 of 12 per 1,000. Hospital Regional Dr. Antonio Musa (HRDAM) is the referral center for 9 public hospitals in the eastern DR and admits approximately 900 neonates to its neonatal intensive care unit (NICU) annually with a mortality rate of about 17%. Providers anecdotally report greater mortality among outborn compared to inborn neonates, but underlying factors that drive differential outcomes have not yet been described in the DR.
Objective:
To describe differences in mortality and risk factors for mortality between outborn and inborn neonates at a regional referral hospital in the DR.
Design/Methods: We reviewed the admission register and medical records for all neonates (≤28 days) admitted to HRDAM NICU from Jun. 1-Nov. 30, 2022. Data were extracted on patient age at admission, sex, birth weight, estimated gestational age (EGA), place of birth, admission diagnosis, and disposition. We used chi-squared or Fisher’s exact tests to compare proportions of outborn and inborn neonates who died, were low birth weight (LBW, < 2500g), and were preterm (EGA < 37 weeks).
Results:
Our sample included 302 inborn and 97 outborn neonates (Figure 1). There was no significant difference in mortality between inborns and outborns (16.6% v 19.4%, p=0.543) (Table 1). Inborns had significantly greater rates of LBW (56.6% v 22.7%, p< 0.001) and preterm birth (48.7% v 32.0%, p=0.001) compared to outborns. Among LBW and preterm infants only, there was a greater disparity in mortality between inborns and outborns, but this still did not reach statistical significance. Compared to inborns, a significantly greater proportion of outborns carried diagnoses related to suspected infection (45.0% v 28.6%, p< 0.001). Finally, we also noted frequent gaps in data reporting for outborns.
Conclusion(s):
We did not detect a significant difference in mortality rates between outborn and inborn neonates at the HRDAM NICU during the study period. However, we did detect significant differences in the prevalence of LBW and preterm between the two populations. While most inborns were admitted for prematurity and related complications, most outborns were admitted for suspected infection. This work highlights potential target areas for improving care and outcomes for outborns. Future work will aim to expand this data set to refine our understanding of drivers of mortality among outborns and identify opportunities for improvement in this referral network.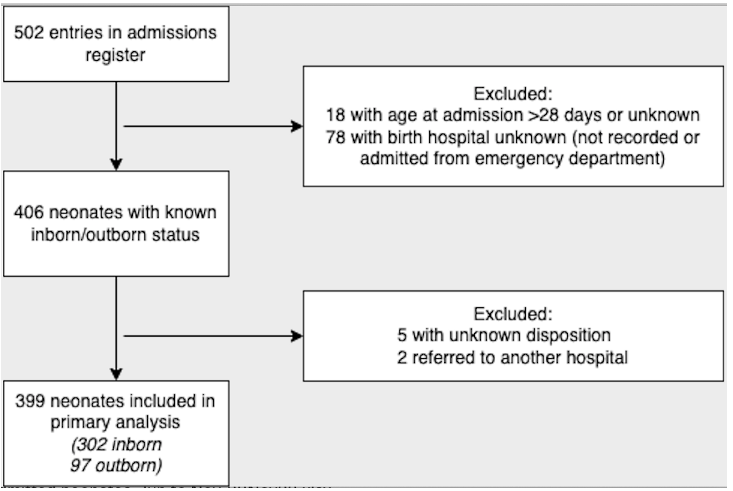
.png)
