Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
708 - Randomized Trial of Effectiveness and Pharmacokinetics of Peripheral Venous vs. Umbilical Venous Epinephrine During Nonatal Resuscitation in Ovine Cardiac Arrest
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 708
Publication Number: 708.445
Publication Number: 708.445
Vidhi Jhaveri, University of California, Davis, School of Medicine, Sacramento, CA, United States; Rebecca Valdez, University of California, Davis, School of Medicine, Davis, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Amy Lesneski, University or California, Davis, Davis, CA, United States; Kirstie C. Tully, University of California, Davis, School of Medicine, Dixon, CA, United States; Payam Vali, University of California, Davis, School of Medicine, sacramento, CA, United States; satyanarayana Lakshminrusimha, UC Davis Children's Hospital, Sacramento, CA, United States; Deepika Sankaran, University of California, Davis, School of Medicine, Sacramento, CA, United States

Vidhi Jhaveri, MD (she/her/hers)
Fellow
University of California, Davis, School of Medicine
Sacramento, California, United States
Presenting Author(s)
Background: Current guidelines recommend umbilical venous (UV) route for epinephrine administration in neonatal cardiac arrest not responding to ventilation and chest compressions. However, UV catheter (UVC) placement can take 5.4 ± 2.2 min (Halling et al 2017) and requires expertise and specialized material that may be a challenge for emergency medical personnel and non-neonatal providers.
Objective: Compare the incidence of return of spontaneous circulation (ROSC) and plasma epinephrine concentrations between low-UVC and peripheral venous (PIV) routes of epinephrine during ovine asphyxial arrest.
Design/Methods: Ten term fetal lambs were intubated and instrumented. Asphyxia was induced by cord occlusion until cardiac arrest. A PIV was placed in a fore limb vein in 5 lambs, and a low UVC was placed to a depth of 2-4 cm in all 10 lambs. Following resuscitation with ventilation and chest compressions, 5 lambs each received epinephrine (0.02 mg/kg) via PIV and low-UVC (2-4 cm) followed by 3-mL saline flush. Hemodynamics and plasma epinephrine concentrations were monitored.
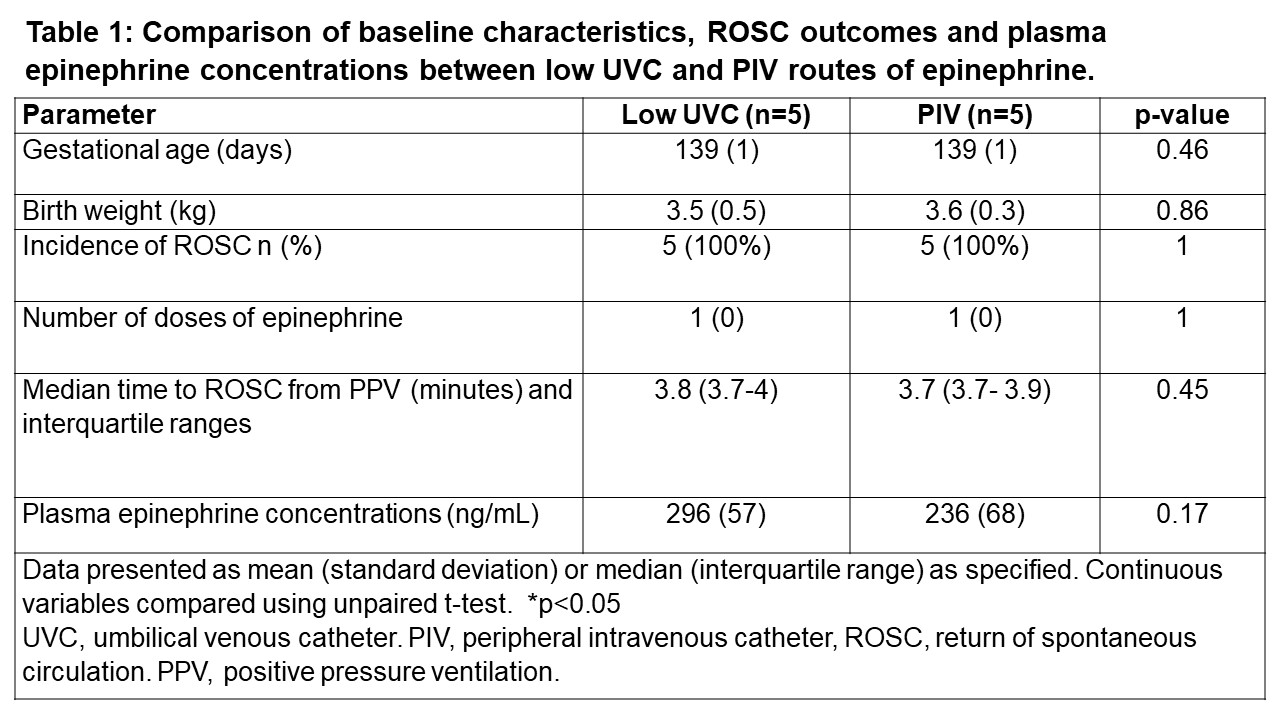
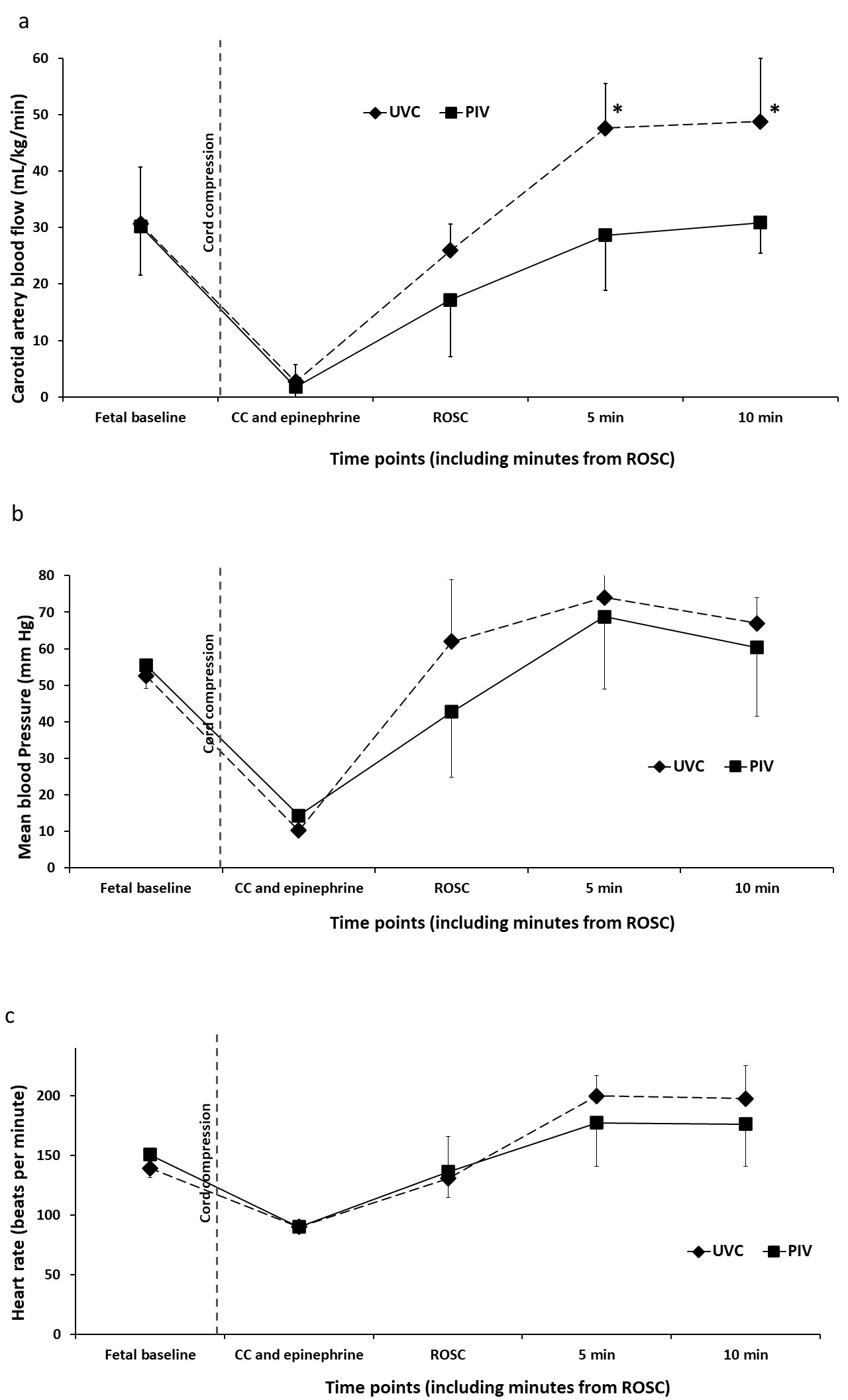
Results: Gestational age and birth weight were similar between the study groups (table 1). All lambs achieved ROSC with the first dose of epinephrine in both UVC and PIV groups (table 1). Time to achieve ROSC was not different between lambs that received UVC vs PIV epinephrine (table 1). Plasma epinephrine concentration at 1 minute after epinephrine administration was similar between PIV and UVC routes (236± 68 vs 296± 57 ng/mL respectively, p=0.17). Carotid blood flow was significantly higher after UVC epinephrine at 5 and 10 min after ROSC (figure 1a). Mean blood pressure and heart rates were similar during resuscitation and after ROSC (figure 1b and c).
Conclusion(s): Incidence of ROSC and plasma epinephrine concentrations were similar between PIV and low-UVC routes. Further studies are warranted to study the feasibility and effectiveness of PIV route of epinephrine in newborns not responding to chest compressions. This simple technique may benefit newborns globally especially when the resuscitator is an emergency medical personnel lacking expertise in UVC placement or in low resource settings without access to UV catheter. Clinical trials to assess the feasibility of placing a PIV in perinatal cardiac arrest to assess the effectiveness of PIV epinephrine are warranted.