Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 4: Surfactant and NIV 1
665 - Role Of The SpO2/FiO2 Ratio As Very Early Indicator Of Success After 1st Surfactant Administration By LISA (1st LISA) In Preterm Infants In NCPAP For RDS
Publication Number: 665.442

Gianluca Lista (he/him/his)
Chief Neonatologist
NICU, V.Buzzi Children's Hospital
V.Buzzi Children's Hospital, ASST-FBF-Sacco
milan, Lombardia, Italy
Presenting Author(s)
Background:
The European RDS guidelines suggest surfactant administration if SpO2< 90% with FiO2 >0.3. Less Invasive Surfactant Administration (LISA) is a largely used new technique to administer surfactant through a narrow catheter during non invasive ventilation (NIV) for RDS. Its safety, effectiveness and outcomes are still debated, especially in very premature newborns.
Objective:
To evaluate the effectiveness, tolerability and long term outcomes of the 1st surfactant administration by LISA in terms of oxygenation and ventilation parameters in the first 24 hours and need for respiratory support and O2 at 36 wks PMA. We also evaluated the role of SpO2/FiO2 ratio after LISA as a indicator of 1st LISA success.
Design/Methods:
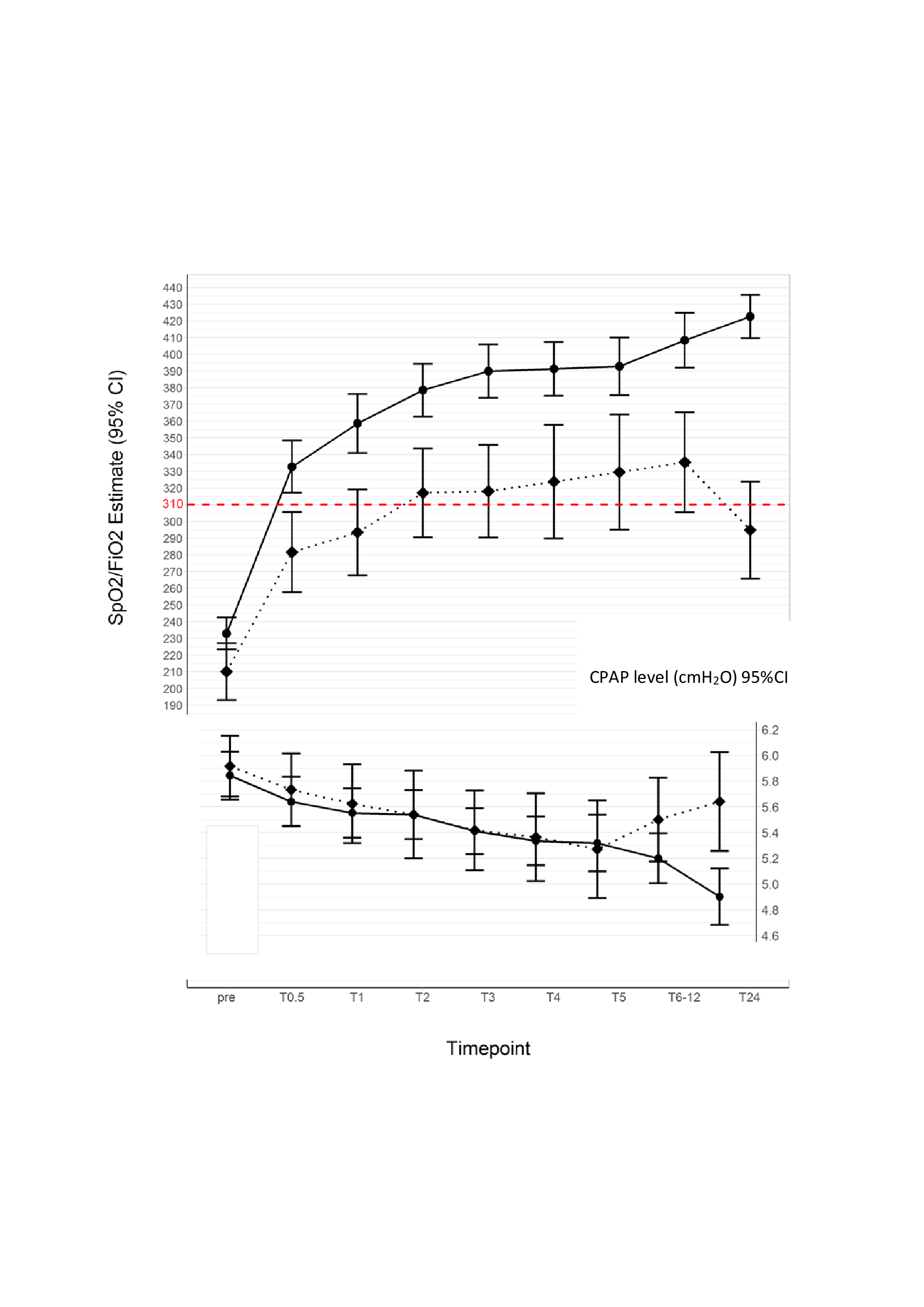
All inborn infants < 37 wks’ GA (March 2014- April 2022) managed from birth with NCPAP for RDS and treated with LISA were included and retrospectically reviewed. We identified two groups: 1st LISA success group (GS no need of surfactant retreatment or intubation within 72 hrs after the 1st LISA) and 1st LISA failure group (GF need of surfactant retreatment or intubation within 72 hrs after the 1st LISA). We compared oxygenation status (SpO2, FiO2, SpO2/FiO2), ventilation (level of CPAP) and respiratory outcomes (length of total respiratory support, NIV, MV and the need for CPAP and O2 at 36 wks) in the two groups. We also studied a SpO2/FiO2 threshold of 310 as a post-manouver indicator of LISA success (corresponding to SpO2 >= 90% and FiO2 < 0.3).
Results:
112 infants (GA 30 wks (28-32), BW 1305g (984-1785) with mild to moderate RDS required LISA within a median of 5 (2-13) hrs of life. Median FiO2 pre-LISA was 0,40 (0,35-0,45). 1st LISA GS and 1st LISA GF showed significant difference in BW, SpO2/FiO2 at 30’ after LISA, CPAP level at 24 hrs, length of any respiratory support and need for CPAP and O2 at 36 wks (Fig 1-2). The multivariate regression showed: SpO2/FiO2 ratio≥ 310 at 30’ after LISA is a indicator of LISA success; the FiO2 level pre-LISA and time from birth-surfactant administration negatively correlate to the achievement of SpO2/FiO2 ratio >=310; a higher FiO2 level pre-LISA and GA at birth< 28 wks correlate with LISA failure (Fig 3).
Conclusion(s):
The success of the 1st LISA (no need of surfactant retreatment or MV within 72 hrs) is significantly associated with better respiratory short and long term outcomes. SpO2/FiO2 >310 at 30’ after LISA predicts success of the manouvre. Moreover, delay in surfactant administration or higher levels of pre-LISA FiO2 negatively affected LISA success with high risk of adverse outcomes.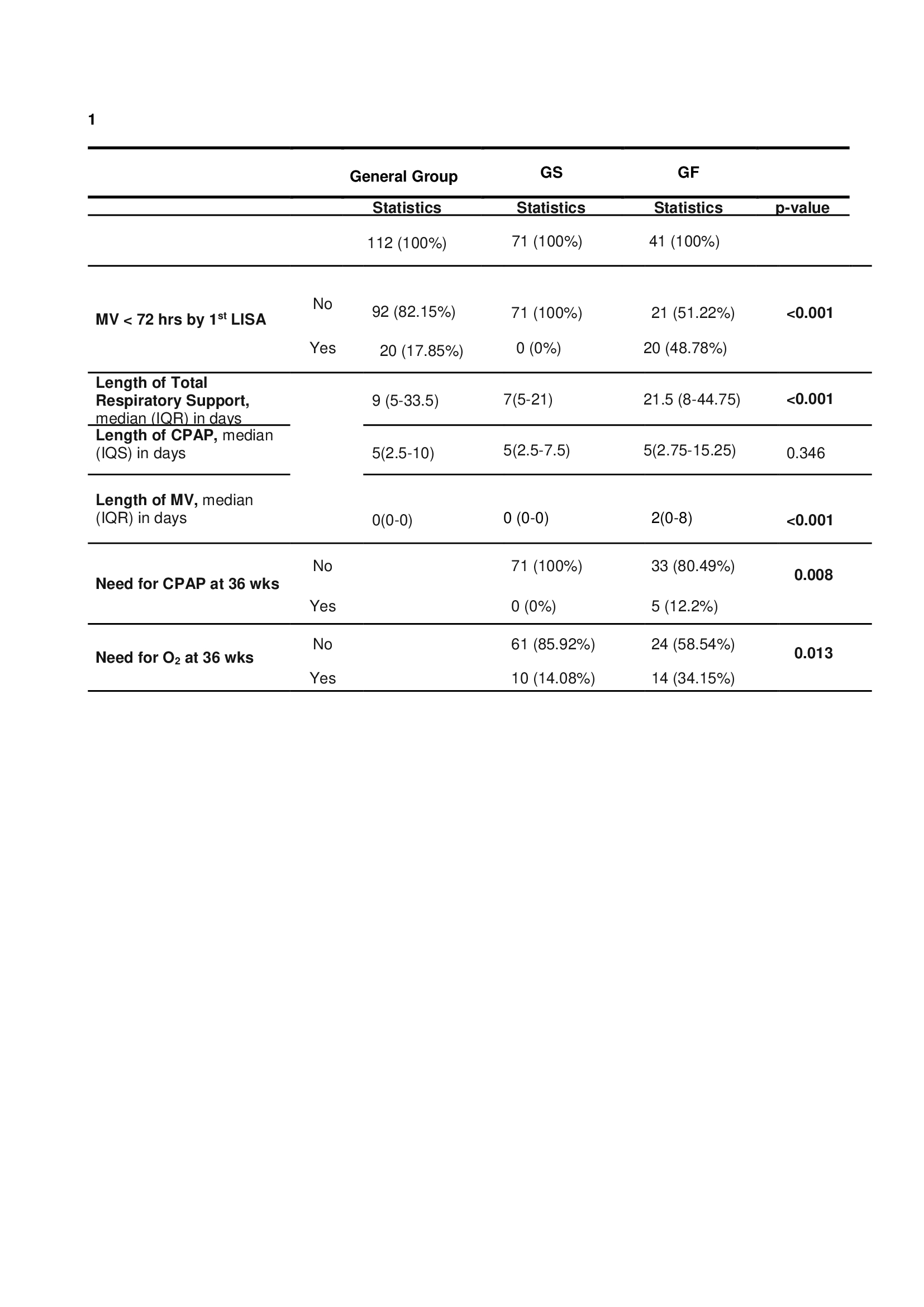
.jpg)
