Neonatal Quality Improvement
Neonatal Quality Improvement 5
197 - A Pilot Project Implementing Eat Sleep Console to Manage Infants with Neonatal Abstinence Syndrome in Women on a Maintenance Assisted Treatment Protocol: An Update
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 197
Publication Number: 197.439
Publication Number: 197.439
Taylor J. Brown, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Jordan Marmet, University of Minnesota Medical School, Minneapolis, MN, United States

Taylor J. Brown, DO (he/him/his)
Fellow PGY-5
University of Minnesota Masonic Children's Hospital
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: In the U.S., the incidence of Neonatal Abstinence Syndrome (NAS) has increased five-fold from 2000-2012 from 1.2 cases per 1000 births in 2000 to 5.8 per 1000 births in 2012. This incidence is a national public health crisis, affecting all regions in the U.S. The variations of care provided for these newborns in the hospital settings contribute to increased hospital stays, high cost of care to families, communities and health care systems. NAS has traditionally been managed with an un-validated Finnegan Neonatal Abstinence Severity Score (FNASS) that and has limited inter-rater reliability. The purpose of this project is to implement a new process known as “eat-sleep-console” (ESC) to decrease in hospital costs, length of stay (LOS) and neonatal opiate treatment exposure.
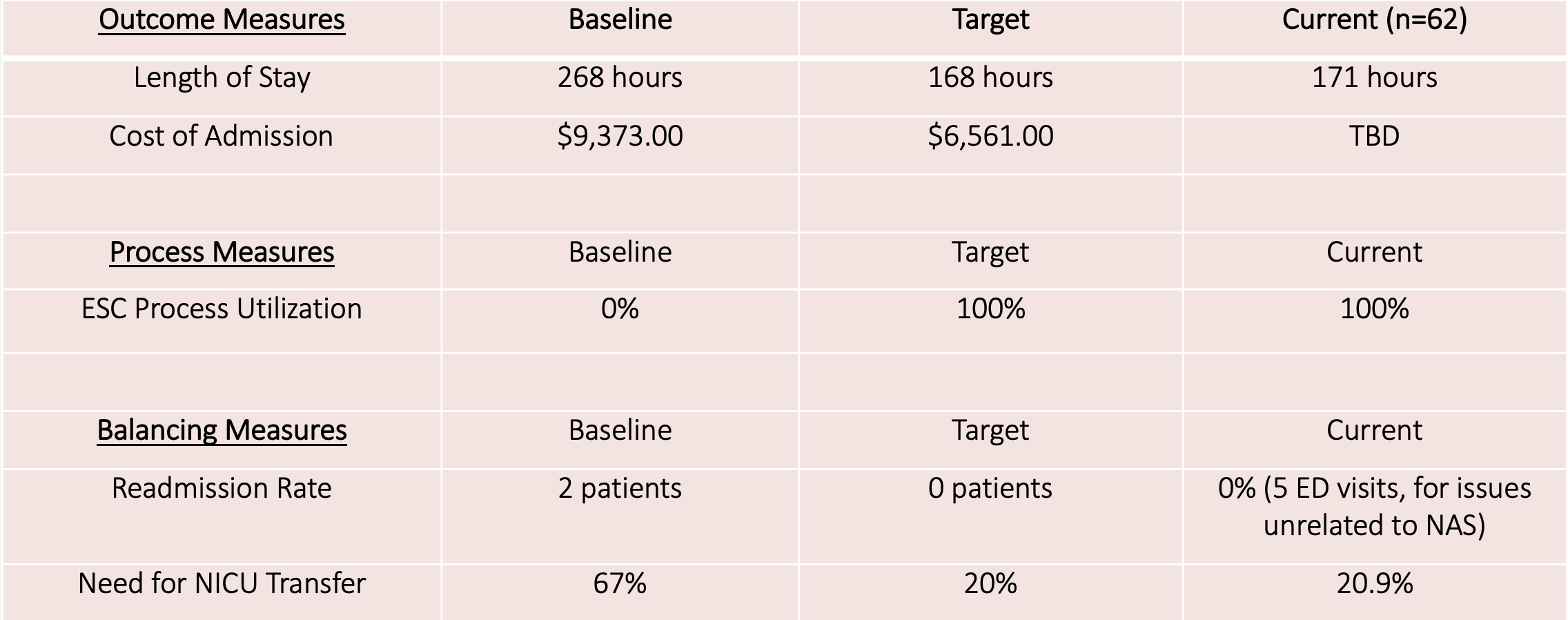
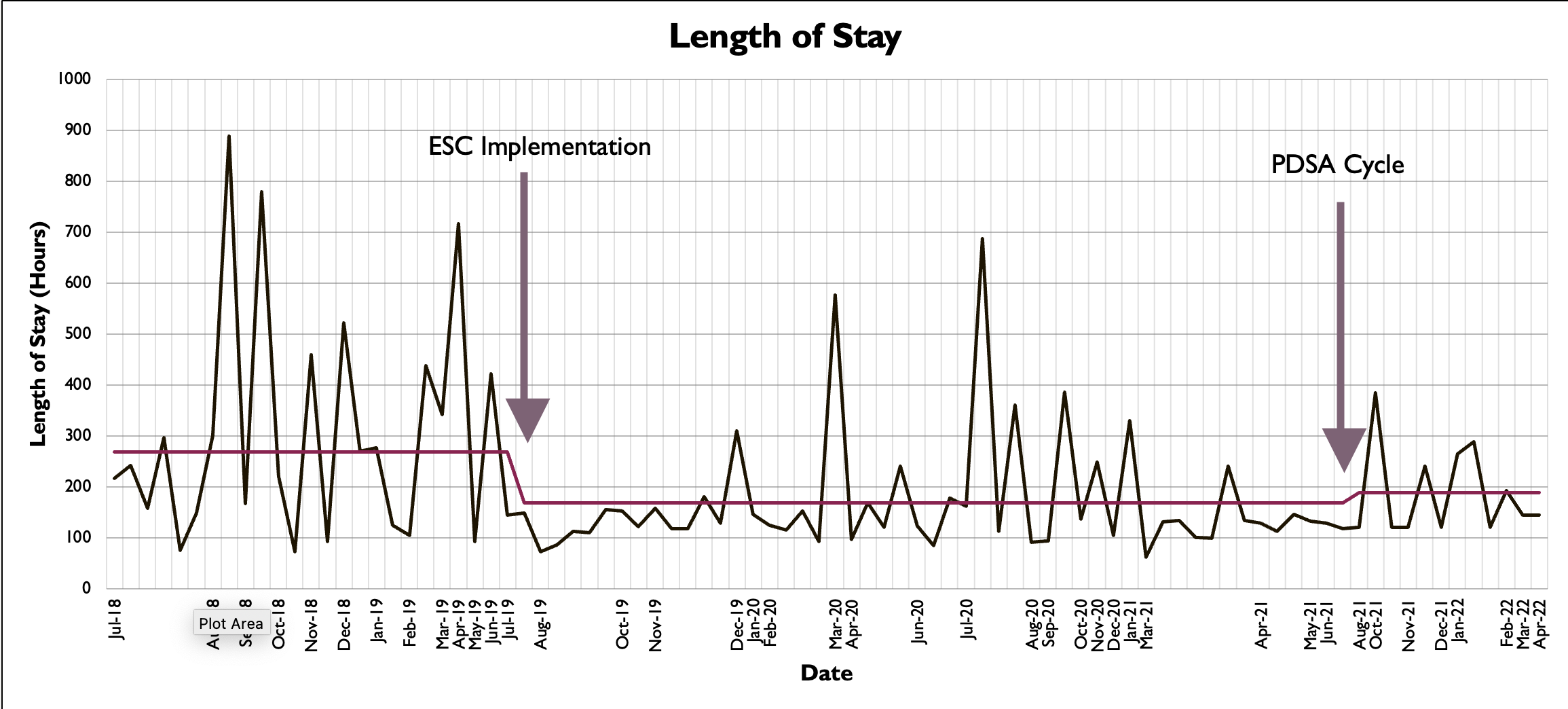
Objective: After implementation of ESC for infants exposed to long acting opioids, we aim to reduce average LOS from 268 hours to 168 hours (7days) as well as decrease cost of admission (COA) by 30%.
Design/Methods: A pilot ESC project was implemented with newborns not admitted to the NICU whose mother was on a medication assisted treatment (MAT) protocol. Patient identification and evaluation algorithms based on the ESC protocol were developed. The medical record was reviewed and LOS, COA, and opioid exposure were collected. NICU transfer and/or return to the emergency department for withdrawal symptoms associated were collected.
Results: 62 newborns have been enrolled in the pilot project from 2019-present. Since implementation, the initial analysis showed a reduction in the average cost of admission, LOS has been reduced from an average of 11 to 7 days, 9 newborns required NICU transfer for withdrawal symptoms unable to be managed by ESC alone, and no readmissions was reported due to NAS.
Conclusion(s): NAS is costly and time consuming to treat. The ESC evaluation protocol is driven by the parent-newborn relationship. The ESC model represents a more cost effective non-pharmacologic model to manage NAS in the hospital setting. Future research and experience is needed to determine additional non-pharmacologic interventions to further alleviate the outcomes of NAS. ESC is reasonable to implement, uses a non-pharmacologic nurse-parent collaborative approach and offers a holistic physiologic care model for nurses, parents and caregivers.