Neonatal Follow-up
NICU Follow Up and Neurodevelopment 6: The NICU Stay and Outcomes
55 - Neonatal Seizures and Associated Neurobehavioral Profiles in Preschool Age Children
Publication Number: 55.446

Allyssa Mattes, PhD (she/her/hers)
Post-Doctoral Fellow
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background:
Neonatal seizures are common in acute brain injury. Up to 25% of survivors develop post-neonatal epilepsy. It is unknown how post-neonatal epilepsy modifies the risk for neurobehavioral challenges following neonatal seizures.
Objective:
We evaluated the relationship between provoked neonatal seizures with or without post-neonatal epilepsy, and adverse neurodevelopmental outcomes including impairments in adaptive, attention, self-regulation, social and emotional function, and sensory processing at preschool age. We hypothesized that a diagnosis of post-neonatal epilepsy by age 24 months would confer greater risk for early markers of neurobehavioral disorders than neonatal seizures alone.
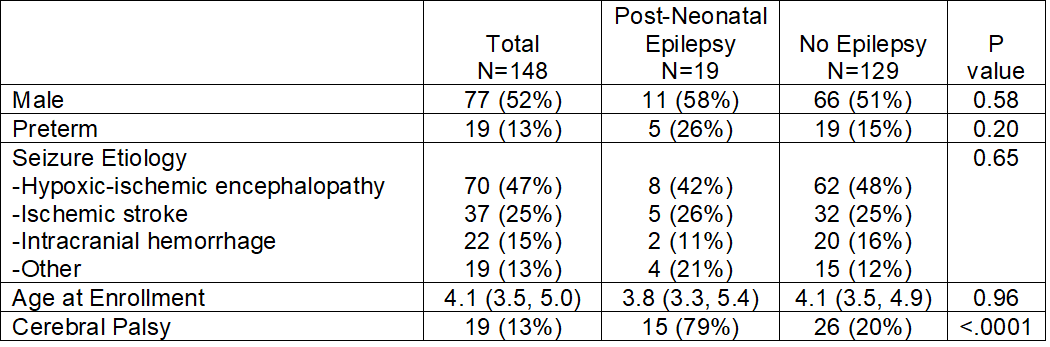
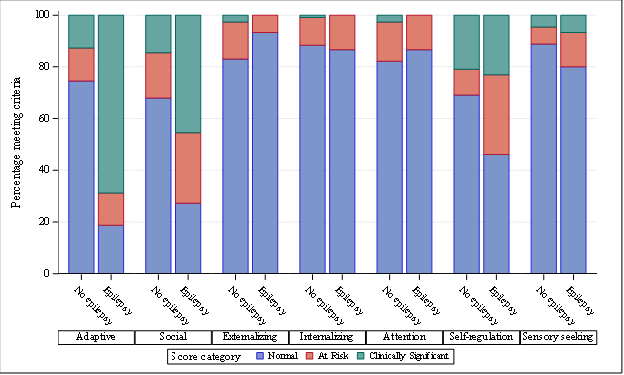
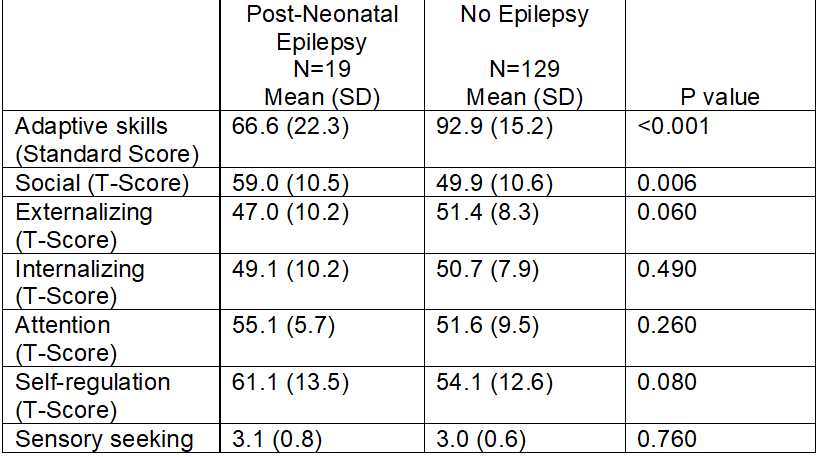
Design/Methods: Neonates with acute provoked seizures born 7/2015-3/2018 were enrolled at 9 Neonatal Seizure Registry sites. Parents completed standardized ratings of adaptive functioning (VABS-3), attention and executive functioning (BRIEF-Preschool; BASC-3), emotional functioning (BASC-3), social skills (SRS-2), and sensory processing (Sensory Profile-2). Composite scores were used to assess Adaptive, Social, Externalizing, Internalizing, Attention, Self-Regulation, and Sensory Seeking domains. We defined “at-risk” scores as 1-1.5 SD from the age-adjusted mean and “clinically significant” scores as >1.5 SD from the mean. Linear regression was used to demonstrate the relationship between composite scores for children who developed post-neonatal epilepsy compared with those who did not. Results were adjusted for neonatal seizure etiology, sex, and gestational age.
Results:
148 children (n=19, 13%, with epilepsy by age 24 months) were enrolled at a median age of 4.1 (IQR 3.5, 5.0) years (Table 1). Clinically significant impairment in adaptive functioning and “at-risk” and “clinically significant” mean neurobehavioral scores were present in several domains (Figure) but only in the epilepsy group. Mean neurobehavioral scores for children without epilepsy were in the average range (Table 2). Risk for neurobehavioral impairment among children with epilepsy persisted after adjusting for seizure etiology, sex, and gestational age at birth.
Conclusion(s): In this multicenter cohort of children who survived provoked neonatal seizures, those who developed epilepsy by 24 months showed higher incidence of adverse neurobehavioral outcomes at preschool age compared with those who did not develop epilepsy. Identifying children at risk for problems with attention, executive function, and socialization is key for developmental support, especially as children graduate from early intervention programs and enter formal schooling.