Quality Improvement/Patient Safety: All Areas
QI 5: Quality Measures, Family Centered & Inpatient QI
247 - Utilizing Change Management Principles to Improve Resident Engagement in a Trainee-led Quality Improvement Project for Family-Centered Rounding
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 247
Publication Number: 247.451
Publication Number: 247.451
Jeremy M. Jones, Children's Hospital of Philadelphia, Philadelphia, PA, United States; John P. Simmons, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Colin J. Crilly, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Sahr Yazdani, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kristin Maletsky, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kim Tran Lopez, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jessica Hart, Childrens Hospital of Philadelphia, Philadelphia, PA, United States
.jpg)
Jeremy M. Jones, MD (he/him/his)
Resident Physician
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
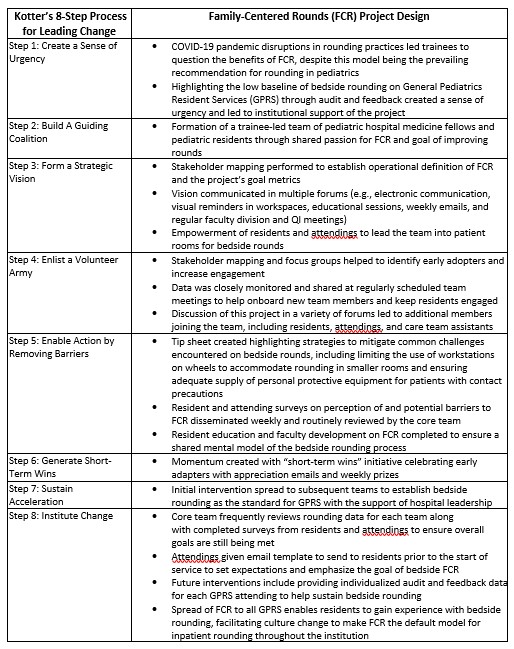
Background: Trainee-led quality improvement (QI) initiatives often struggle to achieve their goals, with the failure to systematically plan for change management (CM) and sustainability as a common cause. Trainees are encouraged to participate in QI projects as part of their professional development, yet many feel disengaged from improvement work due to frequent transitions, limited time, and lack of resources. CM, which is a structured approach that draws on theories from disciplines including psychology, behavioral science, engineering, and systems thinking, can be leveraged to create buy-in from busy trainees. Here, a trainee-led team incorporated Kotter’s “8-Step Process for Leading Change” with conventional QI methodology to increase the percentage of bedside family centered rounds.
Objective: To apply CM principles with the goal of generating sustained resident engagement in a QI project while achieving meaningful improvement in the rounding structure at our institution.
Design/Methods: A group of pediatric residents and pediatric hospital medicine fellows formed a project team. Kotter’s “8-Step Process for Leading Change” was applied as a framework for implementation on a pilot service and then spread across all General Pediatrics resident services (GPRS) (Table 1).
Results: Using a systematic and structured approach, the team successfully built and sustained engagement of residents as well as interprofessional partners including nursing, nonclinical care team assistants, hospital leadership, and patient and family representatives. The resident team has grown from 9 to 16 members (10% of all residents at our institution) with all training levels included. The initiative has been ongoing for 18 months and represents one of the longest and most successful trainee-led QI efforts within the residency program. By leveraging engagement with early adopters, the intervention led to an increase in bedside rounding from 17% to 94% in the pilot unit, and from 4.6% to 55.5% overall after spreading to all GPRS teams.
Conclusion(s): Trainee-led QI projects are at greater risk of failure for a myriad of reasons, including short training periods and positions of lower authority. Incorporating Kotter’s principles of CM with conventional QI methodology successfully led to sustained trainee engagement and acceptance to changes of ingrained institutional rounding practices. Thus, our trainee team demonstrated that utilization of this model ensures systematic consideration of sustainability and is an effective tool when applied to QI to promote trainee-led systemwide culture change and innovation.