Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
705 - Randomized trial of early rapid saline bolus during resuscitation in perinatal ovine hemorrhagic arrest and response to epinephrine
Publication Number: 705.445
- DS
Deepika Sankaran, MBBS MD DCH (she/her/hers)
Assistant Professor of Clinical Pediatrics
University of California, Davis, School of Medicine
University of California, Davis
Rocklin, California, United States
Presenting Author(s)
Background:
Fetal blood loss (e.g. feto-maternal hemorrhage) is a common cause of perinatal asphyxia. In the absence of overt blood loss, diagnosis of hypovolemic arrest in the delivery room can be difficult. It is not known if newborns in severe hypovolemic asphyxial arrest will respond to epinephrine without a volume bolus.
Objective:
Compare the incidence of and time to return of spontaneous circulation (ROSC) between standard neonatal resuscitation (epinephrine before volume bolus over 5min) vs. early rapid (2min) volume replacement before epinephrine.
Design/Methods:
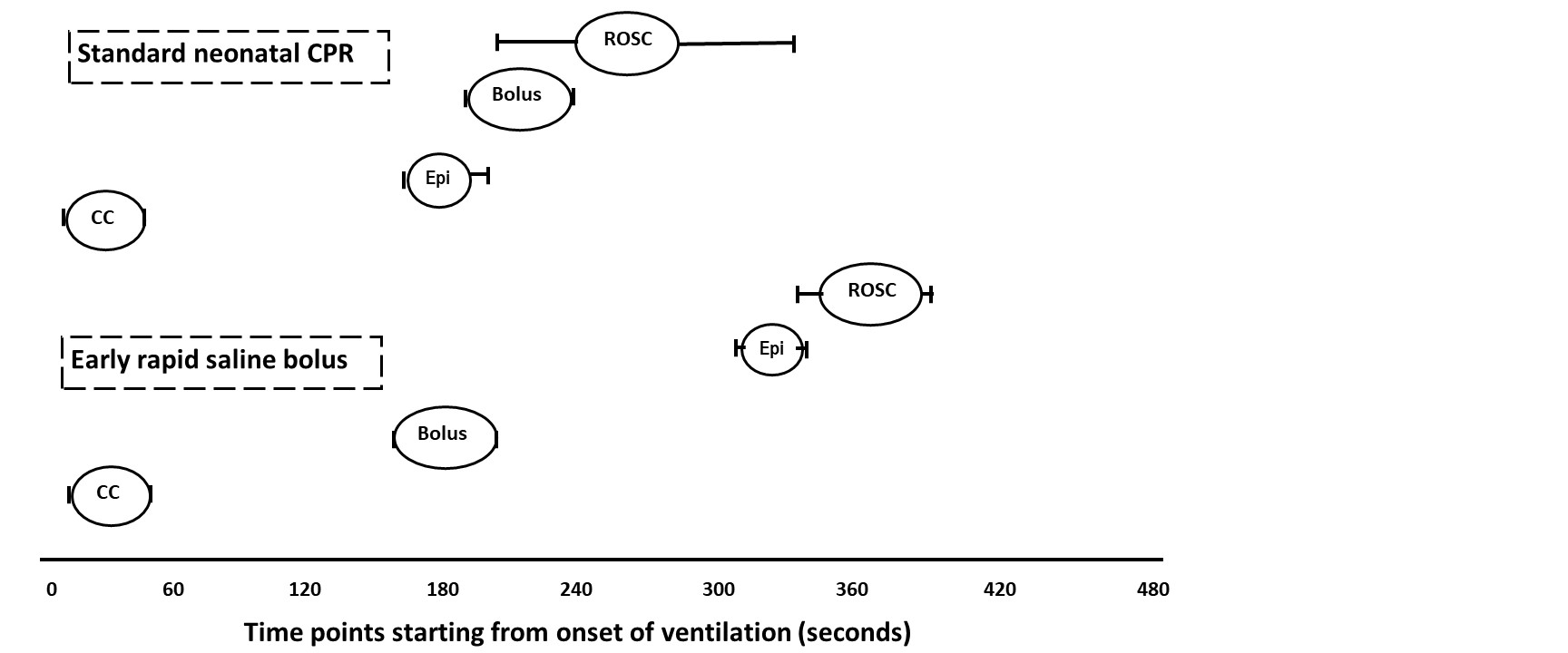
Fetal lambs were intubated and instrumented. Exsanguination (~45-mL/kg) was followed by cord occlusion to induce severe hypovolemia and cardiac arrest. Following 5 min of asystole, term lambs resuscitated with ventilation and chest compressions were randomized to 1) standard neonatal CPR with umbilical venous epinephrine, followed by a 10-mL/kg saline bolus over 5 min if no ROSC, and 2) early rapid saline bolus of 10-mL/kg over 2 min followed by IV epinephrine if no ROSC. Hemodynamics and blood gases were monitored.
Results:
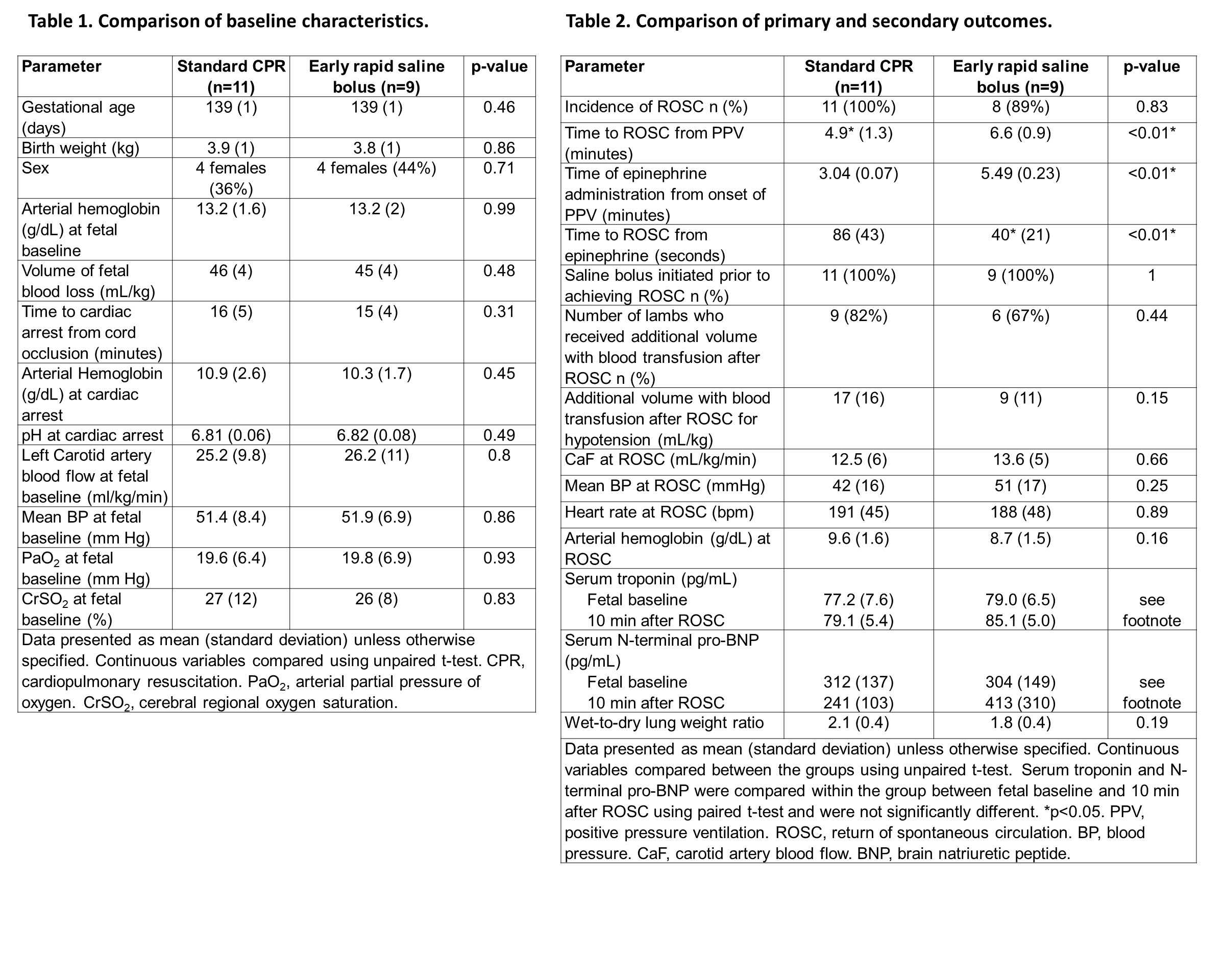
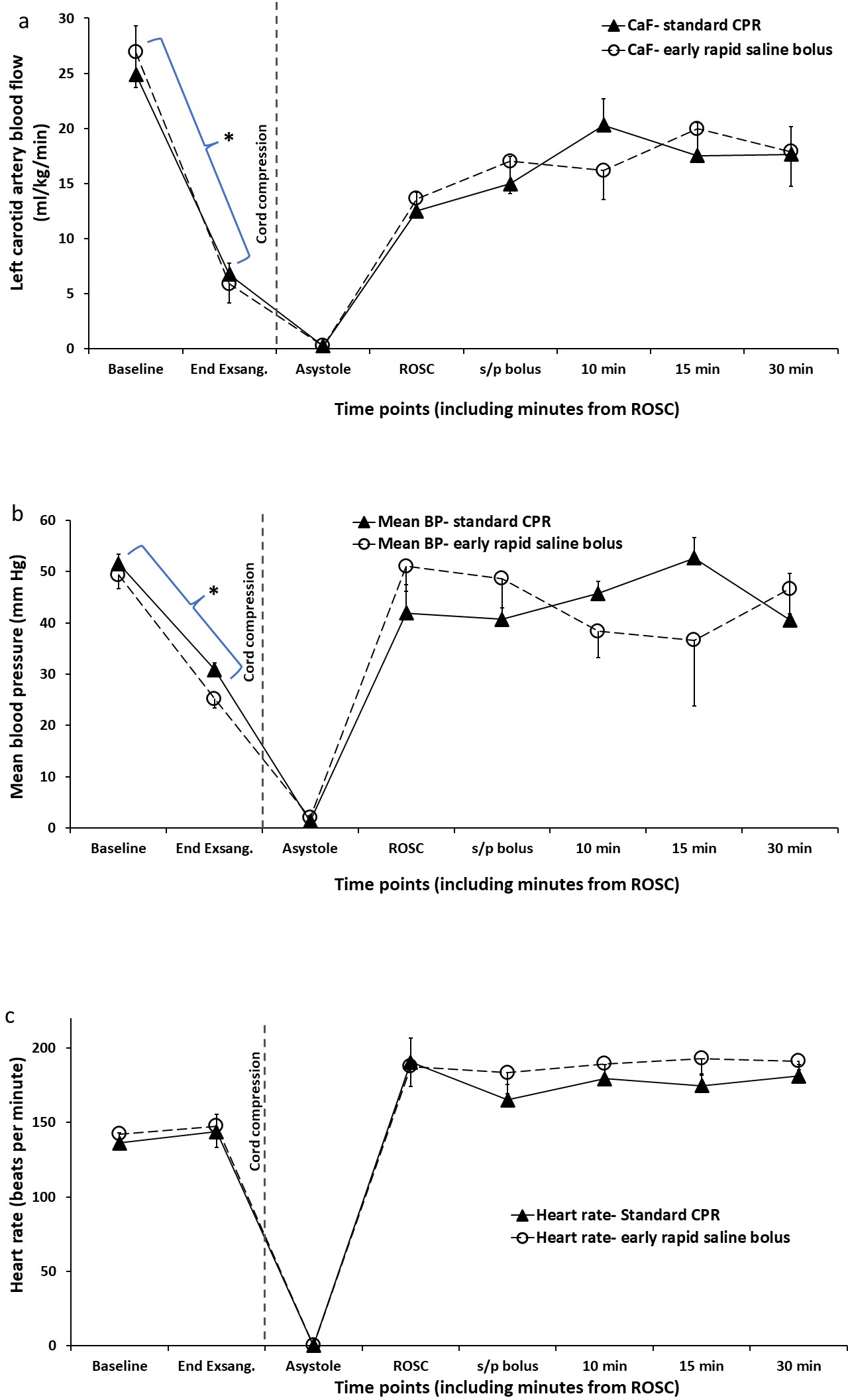
Baseline characteristics were similar between the groups (table 1). In the standard group, epinephrine alone was not associated with ROSC. ROSC occurred after initiation of fluid bolus. In the early saline bolus group, none of the lambs achieved ROSC prior to epinephrine and 8/9 lambs had ROSC after epinephrine. Mean time to ROSC from start of ventilation was shorter in standard CPR (4.9± 1.3 vs 6.6± 0.9 minutes), but time to ROSC from the time of epinephrine administration was shorter with early rapid saline bolus (86± 43 vs 40± 21 seconds, table 2, figure 2). There was no difference in carotid flow, blood pressure or heart rate between the two groups (figure 1). Markers of myocardial stress and pulmonary congestion including serum troponin, pro-brain natriuretic peptide and wet-to-dry lung weights were not different (table 2). Following ROSC, multiple blood transfusions were required to manage systemic hypotension and avoid cerebral hypoperfusion in both groups.
Conclusion(s): Epinephrine alone without volume bolus is ineffective in hemorrhagic arrest. Early rapid saline bolus prior to epinephrine delays administration of epinephrine but shortens time to ROSC after epinephrine. During the post-resuscitation phase, careful clinical assessment of neonatal hemodynamics is critical due to potential need for further volume expansion.