Neonatal Quality Improvement
Neonatal Quality Improvement 7
223 - A Quality Improvement Project to Lower the Incidence of Pneumothorax in Neonates at 36 weeks or Greater Gestational Age
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 223
Publication Number: 223.441
Publication Number: 223.441
Stephen Welty, University of Washington School of Medicine, Tacoma, WA, United States; Jenica J. Sandall, Virginia Mason Franciscan Health, Tracyton, WA, United States
Stephen Welty, MD (he/him/his)
Clinical Professor of Pediatrics
University of Washington School of Medicine
Tacoma, Washington, United States
Presenting Author(s)
Background: Our Nursery at Saint Joseph Medical Center is a referral level 3 nursery in Tacoma Washington that has a delivery service with approximately 4000 deliveries/yr, and is a referral center for the Virginia Mason Franciscan Health System in the Puget Sound Region. We have submitted our outcomes data to the Vermont Oxford Network since 2014. We noted that from 2014 to 2016 that the number of term neonates admitted to our nursery with symptomatic pneumothoraces had steadily increased so that in 2016 more than 10% of admissions 37 weeks or greater were diagnosed with a pneumothorax. In August of 2017 we implemented a new respiratory care algorithm in the delivery room designed to reduce the incidence of symptomatic pneumothorax in term neonates.
Objective: To lower the incidence of pneumothorax in term neonates by implementation of a respiratory care guideline in the delivery room that deemphasized the aggressive use of continuous positive airway pressure (CPAP) in the delivery room.
Design/Methods: We reviewed potentially better practices for delivery room management of term neonates with respiratory symptoms and noted the following.
1. The seventh edition of NRP was interpreted by practitioners to emphasize CPAP utilization in the delivery room.
2. Reports of increased rates of pneumothoraces associated with high rates of delivery room CPAP suggested that this practice may increase the risk for pneumothoraces
The following PDSA cycles were done.
1. PDSA 1 was to create a data collection tool so that rates of CPAP utilization in the delivery room could be assessed easily.
2. PDSA 2 was to create an NRP algorithm that deemphasized the aggressive early use of CPAP in the delivery room (Figure one)
3. PDSA 3 was to have broad based interdisciplinary education to the implementation of the algorithm.
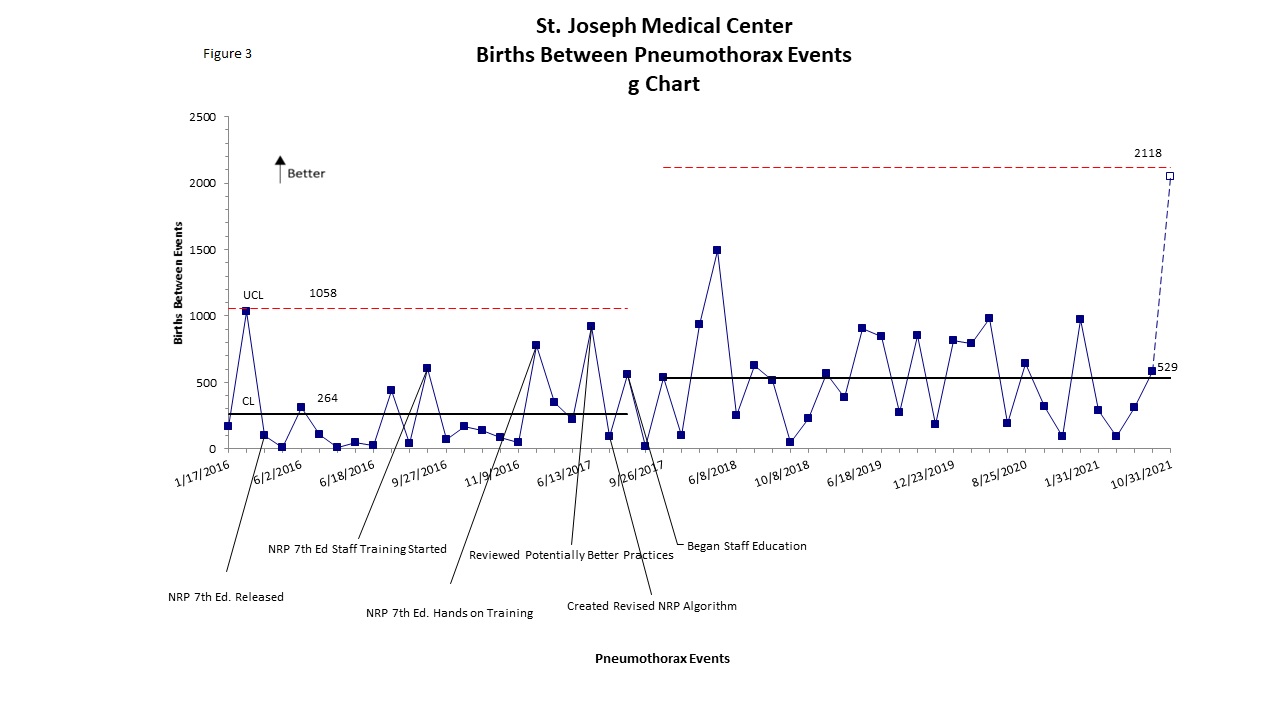
We utilized G charts to assess deliveries at 36 weeks or greater gestational age between events. We utilized a P chart to assess the proportion of these neonates receiving CPAP or PPV. Our primary balancing measure was to determine whether admissions for respiratory diagnoses was increased.
Results: After implementation of the NRP guideline the rates of utilization of positive pressure in the delivery room decreased from 4.8 to 3.0%. The number of deliveries between event increased from 264 to 529. There was no increase in neonates admitted to the nursery with a respiratory diagnosis (3.1 to 2.6% pre and post implementation).
Conclusion(s): Implementation of a NRP guideline that deemphasized the use of CPAP in the delivery room was associated with a decrease in the incidence of pneumothoraces in term neonates.
.jpg)
.jpg)