Quality Improvement/Patient Safety: All Areas
QI 4: Inpatient QI/Patient Safety
234 - Choosing Wisely for Bronchiolitis Amid a Respiratory Surge
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 234
Publication Number: 234.45
Publication Number: 234.45
Daniel P. Schlepphorst, Levine Children's Hospital, Charlotte, NC, United States; Marybeth A. Burriss-West, Levine Children's Hospital, Charlotte, NC, United States; Kyle Barnack, Levine Children's Hospital, Charlotte, NC, United States

Daniel P. Schlepphorst, D.O. (he/him/his)
Resident Physician
Levine Children's Hospital
Charlotte, North Carolina, United States
Presenting Author(s)
Background: Bronchiolitis, a viral lower respiratory tract infection, is a leading cause of pediatric emergency department (ED) visits and hospitalizations. The American Academy of Pediatrics (AAP) and Society of Hospital Medicine (SHM) recommend reliance on history and physical exam to diagnose bronchiolitis. Studies show that use of chest x-rays, bronchodilators, antibiotics and steroids have limited utility in diagnosis and treatment of uncomplicated bronchiolitis. While the AAP and SHM “Choosing Wisely” initiative recommends avoiding these interventions to reduce unnecessary exposures and costs, many providers struggle to follow the guidelines. We improved adherence to the guidelines at our institution through methods discussed below. After sustaining our goal and shifting the median, we now face new obstacles amidst the ongoing respiratory surge, which provides a real-time glimpse of factors that influence provider practice. At LCH, our providers began trialing albuterol on patients in respiratory distress regardless of suspected etiology as an effort to reduce admissions.
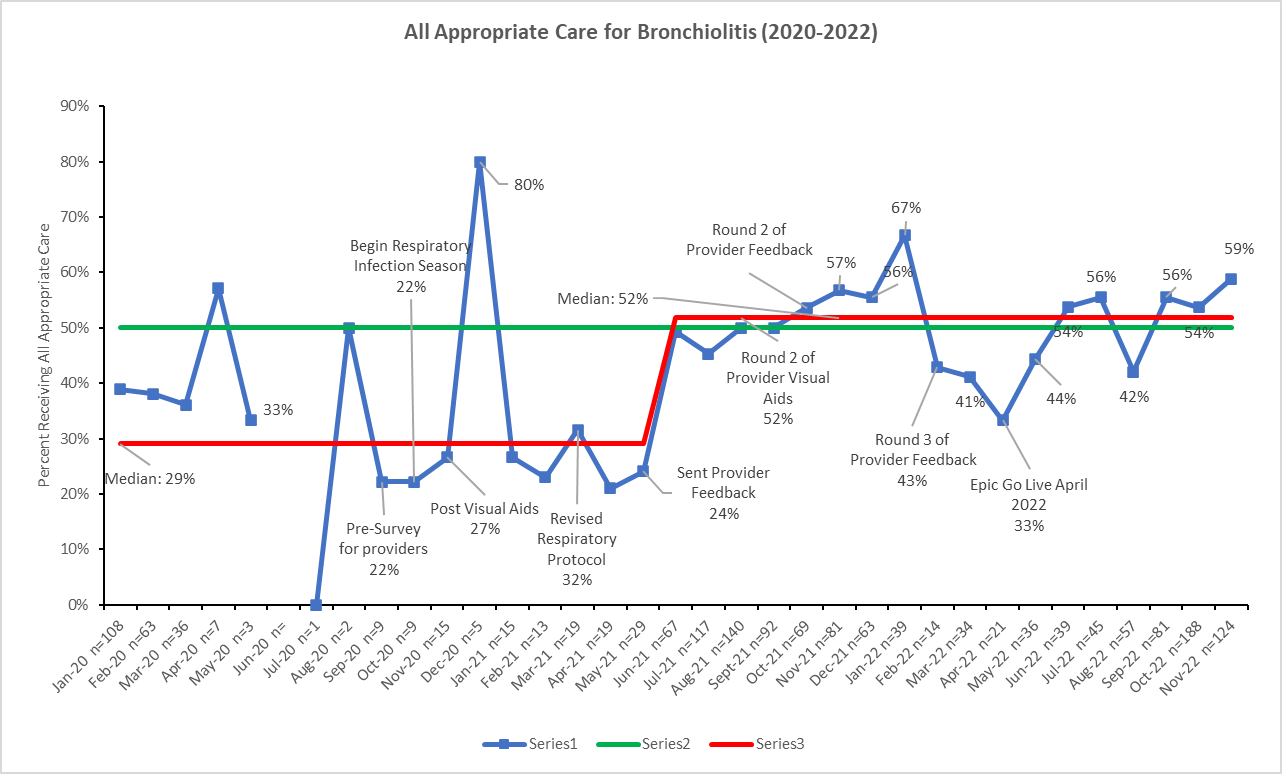
Objective: The aim of this QI project is to reduce unnecessary interventions, thus providing high-value care for children aged 2 months to 2 years with bronchiolitis within the ED and hospital. We met our goal adherence rate to the Choosing Wisely guidelines (Patients receiving zero of the select interventions) of 50% by May 2022, and interestingly, maintained this goal during the respiratory surge.
Design/Methods: This project used the Model for Improvement and employed rapid plan, do, study, act (PDSA) cycles. The multi-disciplinary team is composed of physicians, respiratory therapists (RT), nurses and QI coaches. PDSA change concepts included knowledge surveys, visual aid campaigns, modification of order sets, altered RT protocols, resident education sessions and individualized provider feedback on comprehensive use of the above Choosing Wisely interventions.
Results: Following provider education and individualized provider feedback, a sustained shift occurred in the median bundle performance from 32% to 50%, achieving our goal in Fall 2021. We continued to meet our goal during the respiratory surge despite the hospital-wide trend to trial albuterol.
Conclusion(s): Changing practice patterns to meet evidence-based standards is challenging. Lack of provider familiarity with the Choosing Wisely recommendations presented an opportunity for improvement. Education, decision support tools, visual aids, and individual performance feedback proved to be helpful to overcoming barriers to change, and hopefully will help maintain these practices.