Pulmonology
Pulmonology
173 - Implementing High-Tech Homecare in the Amish Community: Experience with Chronic Respiratory Failure in Infants with Ellis-Van Creveld Syndrome (EVC)
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 173
Publication Number: 173.449
Publication Number: 173.449
Aaron Chidekel, NemoursAlfred I. duPont Hospital for Children, Wilmington, DE, United States; Devyani Chowdhury, Nemours Children's Hospital, Hershey, PA, United States; Melissa Olsakowski, Nemours Children's Hospital, Wilmington, DE, United States; Laura E. Poskitt, Clinic for Special Children, Strasburg, PA, United States
Aaron Chidekel, MD (he/him/his)
Chief, Division of Pulmonology and Sleep Medicine
NemoursAlfred I. duPont Hospital for Children
Wilmington, Delaware, United States
Presenting Author(s)
Background: EVC is an autosomal recessive chondroectodermal dysplasia common in the Lancaster County Amish community. EVC is characterized by polydactyly, congenital heart disease and restrictive lung disease of varying severity.
Objective: To review the implementation and delivery of high-tech homecare among Amish infants with EVC and chronic respiratory failure (CRF).
Design/Methods: As part of an IRB-approved retrospective study reporting long-term pulmonary outcomes of EVC and CRF, from January 2007 to the present, the implementation and delivery of multidisciplinary high-tech homecare in Amish infants was reviewed. Issues unique to this population were identified and strategies to deliver safe and effective long-term care characterized.
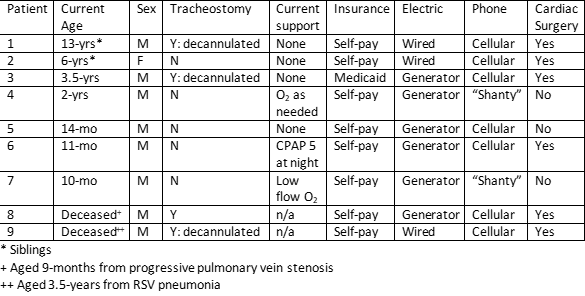
Results: The cohort consists of 9 infants (8 male) with EVC in 8 households (7 self-pay, 1 Medicaid). All required long-term mechanical ventilation via tracheostomy (N=4) or non-invasive positive pressure ventilation via RAM cannula (N=5). Patients with tracheostomy had suction machines and home "nursing" provided by trained Amish caregivers. All infants had O2 concentrators, continuous monitoring by pulse oximetry, supplemental feeds with pumps, and nebulizers and compressors for inhaled medications. 2 families of infants with tracheostomy brought alternating current electricity into in a single room in their home. Six families used portable propane generators to provide electricity. These families charged batteries to minimize generator use and used an inverter. Most families also had 1 or 2 solar panels. A single homecare equipment company provided service to all families. No family had a landline telephone. Two households had a telephone in a "shanty" on their property; the others used cellular telephones intermittently. The medical team provided personal cellphone numbers to facilitate communication. Safe and timely follow up was coordinated between the pediatrician, cardiologist and pulmonologist and delivered through home visits and multidisciplinary appointments at the Clinic for Special Children. Visits with individual providers were enhanced by real time videoconference with other team members. Families were accepting of medical technology in the context of improved outcomes for EVC. Families welcomed home visits and felt they enhanced safety and efficiency and reduced costs associated with hiring drivers for appointments.
Conclusion(s): High-tech home care is feasible in the Amish community with careful planning to meet the unique needs of this population. Communication and care coordination strategies can be adapted to provide safe, effective multidisciplinary care.