Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
696 - Provider-selected bed height improves ergonomics and chest compressions performance during simulated neonatal resuscitation
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 696
Publication Number: 696.445
Publication Number: 696.445
Tamara Alexander, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Courtney N. Massey, Oklahoma Childrens Hospital at OU Health, Oklahoma City, OK, United States; Leonard W. Wilson, University of Oklahoma Health Sciences Center, CHOCTAW, OK, United States; Lise DeShea, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; William H. Beasley, University of Oklahoma HSC, Norman, OK, United States; Szyld Edgardo, University of Oklahoma College of Medicine, oklahoma city, OK, United States; Carol P. Dionne, University of Oklahoma College of Allied Health, Albuquerque, NM, United States; Birju A.. Shah, University of Oklahoma Health Sciences Center, Oklahoma City, OK, United States
.jpg)
Tamara Alexander, MD (she/her/hers)
Neonatal Perinatal Medicine Fellow
University of Oklahoma College of Medicine
Oklahoma City, Oklahoma, United States
Presenting Author(s)
Background: Chest compressions (CCs) are rare during neonatal resuscitation in the delivery room (DR) with 0.1% of term infants and up to 15% of preterm infants needing CCs if their heart rate falls below 60 beats per minute. Evaluation of human factors is needed to understand the determinants of effective performance of CCs. Resuscitations take place in the DR on a neonatal warmer at a standard height. Despite the provider’s ability to adjust the warmer height, few change the position, which may affect the quality of CCs.
Objective: To use kinematic 3-D motion analysis during simulated neonatal resuscitation to evaluate changes in depth, force, and rate of CCs between provider-selected bed height versus a standard bed height.
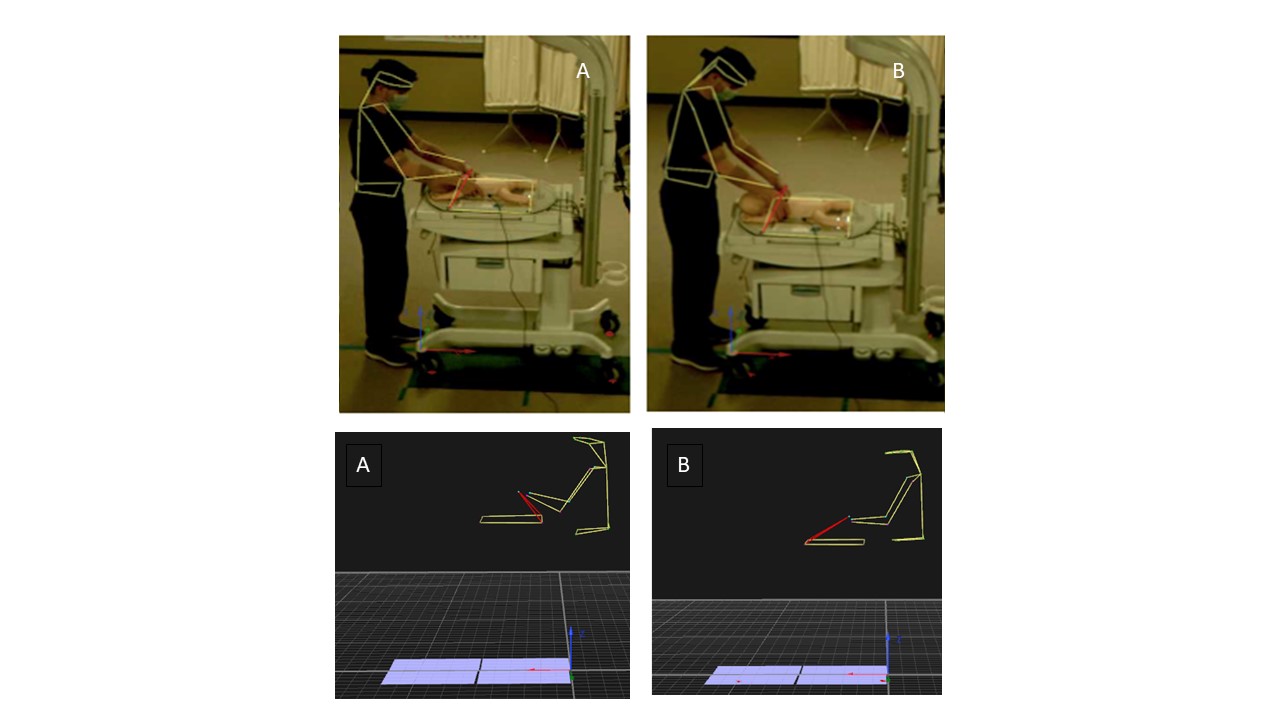
Design/Methods: Institutional review board (IRB) approved informed consent was obtained. A convenience sample of 20 Neonatal Resuscitation Program (NRP)-trained providers participated in a crossover simulation study of neonatal manikin CCs with a 10-min rest between each 10-min simulation. The order of conditions (standard versus provider-selected height) alternated by participant. Participants had reflective markers applied to anatomic landmarks that created a motion capture model continuously analyzed (Figure 1). A lab technician asked for ratings of perceived exertion every 2 min. Statistical analysis was completed using linear mixed-effects models with subjects as a random factor.
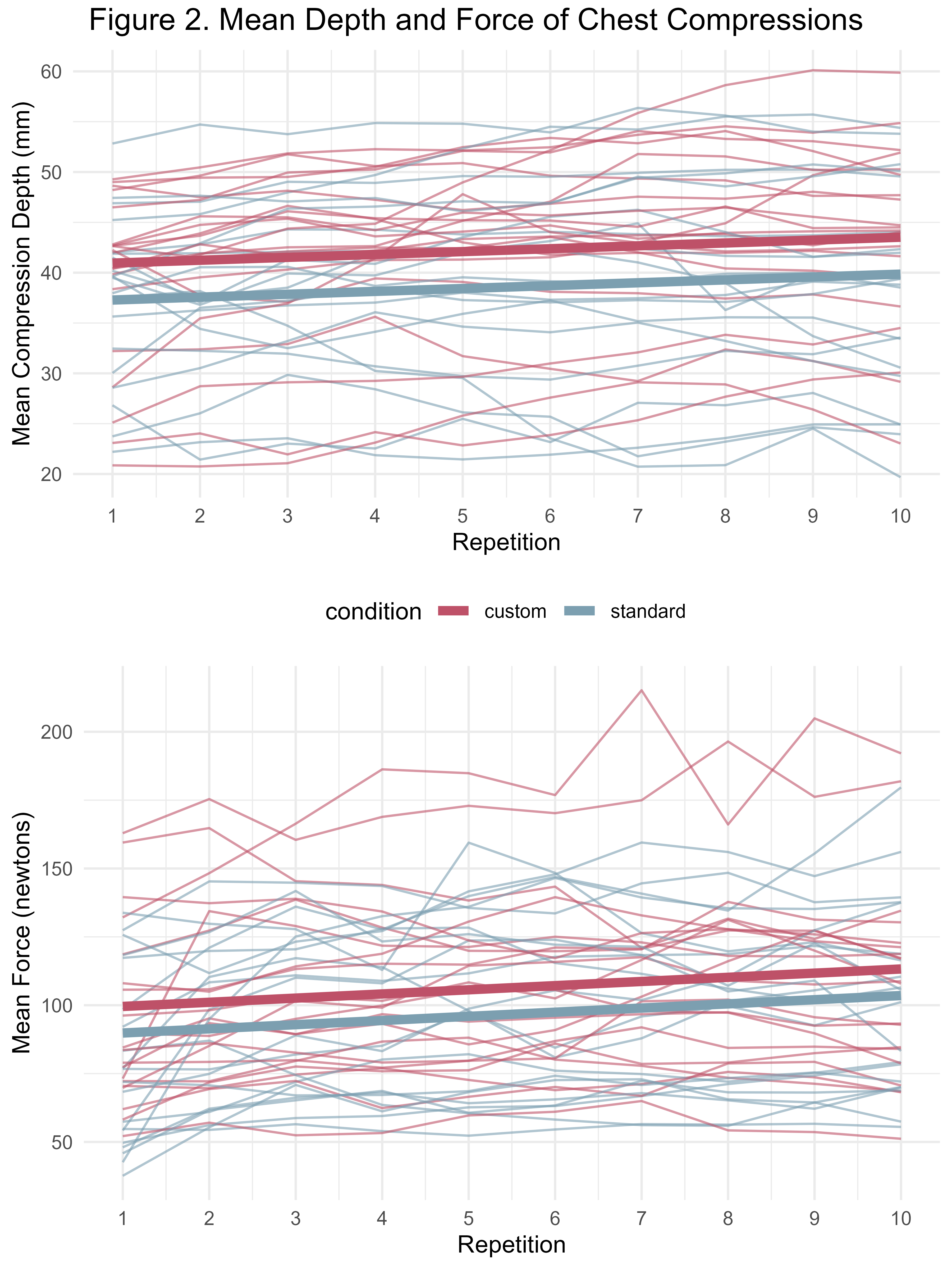
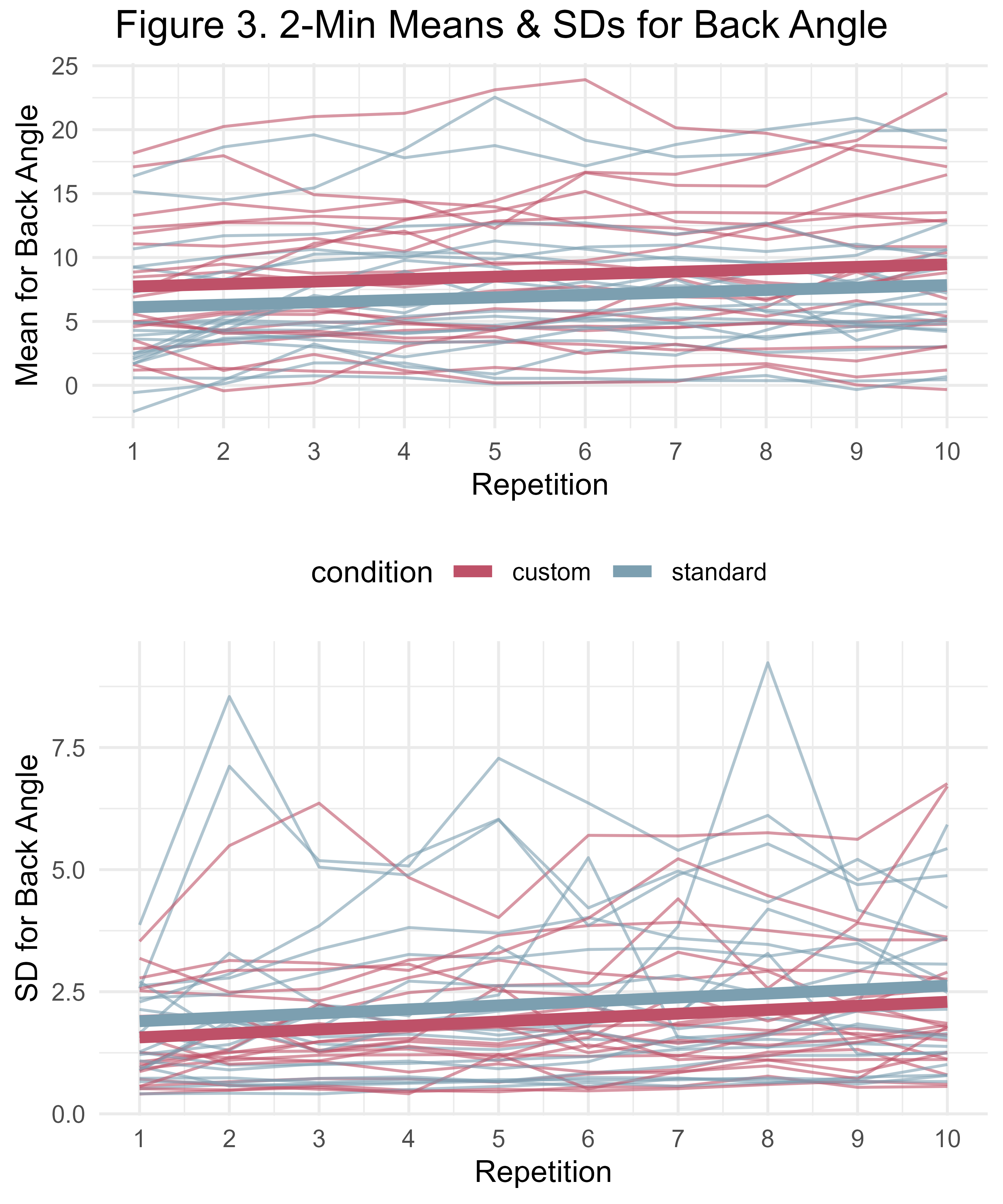
Results: The 12 women and 8 men included nearly equal numbers of participants in the normal, overweight and obese categories. Nineteen providers (95%) lowered the warmer (M = 91.7 cm, SD = 4.9) from the standard 100-cm height. The mean depth and force of CCs significantly increased over the course of each simulation (p < .05) with custom height having significantly higher means than the standard height (p < .05) (Figure 2). The rate of chest compressions did not differ significantly between conditions or throughout the simulation. Providers reported significantly less fatigue in the custom condition than standard condition, based on the Borg Rating of Perceived Exertion scale; scores increased significantly during the simulations. The variation of back angle, measured by the standard deviation estimated every 2 min, significantly increased over the course of each simulation (p < .05), with the standard condition having significantly greater variation than the custom condition (p < .05) (Figure 3).
Conclusion(s): Our data suggests adjusting the bed height to the providers’ preference leads to improved quality of chest compressions and less fatigue during simulated neonatal resuscitation.